World Nutrition
Volume 4, Number 3, March 2013
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary. Fortification. Folic acid and spina bifida
Is it safe? Is it wise?
Is it right?

Access pdf of this commentary here
Access pdf of this month's WN editorial here

Mark Lawrence
Population Health Strategic Research Centre
Deakin University, Melbourne, Australia
Email: mark.lawrence@deakin.edu.au
Folic acid fortification

Food fortification is very powerfully advocated and commonly practiced worldwide, as celebrated here in South Africa (left) and in the USA (right)
Food fortification takes many forms. The example discussed here is unusual, because in many countries now it is required by law: the fortification of flour with the B vitamin folic acid, or MFFFA for short. Voluntary fortification of various food products was first used to help prevent and control child and maternal anaemia associated with folate deficiency (1). In the mid-1990s, policy-makers in various countries began considering using mandatory fortification under a novel policy paradigm, that fortification was needed to increase the folic acid intake and protect the health status of people who had a special requirement for this nutrient, irrespective of the folate status of the population as a whole.
The new policy view was prompted by the need to respond to convincing epidemiological evidence that increasing folic acid intake for vulnerable women reduced their risk of having a neural tube defect-affected pregnancy. These defects are malformations of the central nervous system resulting from the failure of the neural tube to close during embryogenesis. They most commonly include spina bifida and anencephaly. When the child survives, such defects place a devastating health, social, financial, and emotional burden on affected people and their families. National neural tube defect birth prevalence varies widely. In the 1970s, rates of up to and even above 10 per 1,000 live births were recorded in Scotland, Ireland and Wales (2). More recently rates up to 6 per 1000 live births have been recorded in China (3). Over 95 per cent of all cases are first occurrence, with a small proportion being recurrent events in women with a previously affected pregnancy (4).
Mandatory flour fortification with folic acid (MFFFA) remains a vexed and controversial policy option. It is associated with many scientific uncertainties and ethical dilemmas. In responding to the epidemiological evidence, policy-makers have struggled to formulate a policy that promotes the health interests of those who are most at risk, while protecting the health of the wider population. David Kessler, the commissioner of the US Food and Drug Administration when fortification was debated in the US, saw the mandatory option as medicalisation of the food supply.
For scholars and policy-makers, the issues surrounding mandatory folic acid fortification are especially interesting. At the time it was first being implemented, an authority on the topic, also the editor of an international nutrition journal, described the relationship of folic acid to neural tube defects as providing 'one of the richest case studies in nutrition science policy of this half century'(5).
In response to concerted appeals for action, and specifically for mandatory fortification, the World Health Organization and the UN Food and Agriculture Organization eventually published guidelines on levels of folic acid fortification for wheat and maize flour. They recommended fortification at levels of 1.0 to 5.0 parts per million, depending on a country's average per head wheat flour consumption (6).
Box 1
Issues of fortification
Editor's note. The commentary published here is a condensed version of one chapter in the new book Food Fortification. The Evidence, Ethics and Politics of Adding Nutrients to Foods, by Mark Lawrence, now published by Oxford University Press. The book examines the opportunities and problems arising from the fortification of food ingredients and products using synthetic nutrients, whose stated purpose is improvement of the quality of food supplies, so as to protect health, in particular of unborn children.
Food product and ingredient fortification is an important public health nutrition issue. Foods and food products have been fortified beginning almost a century ago, ever since various micronutrients began to be identified and isolated and their functions understood. Usually the term 'fortification' is taken to mean the addition of a synthetic nutrient at levels different from those found in the food, product or ingredient itself. 'Enrichment' is usually taken to mean the replacement or partial replacement of a nutrient that has been depleted in the process of manufacture, or else to make the product nutritionally equivalent to an alternative. Mandatory policies are not new: thus, milk, white bread and margarine are by law, fortified or enriched in many countries. 'Supplementation' usually refers to the use of synthetic nutrients in the form of powders, pills or liquids, typically to treat deficiency diseases or to protect against deficiency in vulnerable populations.
Fortification and enrichment are contentious strategies. Fortification is a powerful public health policy tool. Fortification of ingredients and products with synthetic versions of a large number of micronutrients is supported by regulatory bodies, relevant UN agencies, foundations and other funders, aid organisations, the research science community, the food and product manufacturing industry, governments, and other actors. Usually, fortification is voluntary, in the sense that manufacturers are free to fortify or not, in which case customers can make choices.
Fortification is however, a contentious policy. It may encourage consumers to choose an inferior product instead of one that is a naturally better source of nutrients. White bread is an example. It is liable to be instituted without the fully informed consent of consumers. Fortification of flour with folic acid, the story told here, is an example. It could result in products or diets that are undesirably unbalanced. This may be an issue only when potentially toxic nutrients are used. Because manufacturers are entitled to make health claims for fortificants in their products, they may lead to sustained or increased consumption of fatty, sugary or salty fortified products. Breakfast cereals are an example.
Extensive use of fortification in low-income countries is criticised as a diversion from the longer-term task of making food supplies secure and naturally good sources of nutrients from culturally appropriate foods suited to the local climate and terrain. Some critics object to mandatory fortification on principle, as an inappropriate 'medicalisation' of food supplies. All these issues are addressed in Mark Lawrence's new book.
The 1990s
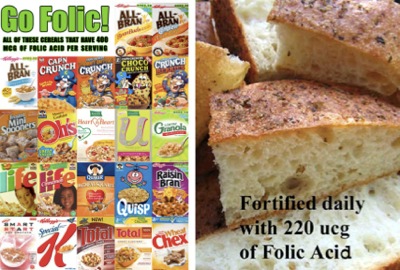
Where policy on folic acid has led. Breakfast cereals fortified voluntarily, and flour used in bread manufacture as now mandated by law in many countries
The impetus for policy-makers to consider mandatory fortification was the publication of the findings from trials reporting the protective effect of folic acid supplements for the occurrence and recurrence of neural tube defects (7,8) in the early 1990s. Shortly after these studies were published, the US Centers for Disease Control and Prevention recommended that all women of childbearing age consume 400 micrograms of folic acid daily (9). Similar recommendations followed shortly thereafter in many countries around the world. Commonly, this involved recommending a 400 microgram folic acid supplement daily to all women planning pregnancy and ten times that amount – 4 milligrams – to those with a previously affected pregnancy. Voluntary folic acid fortification was permitted in many countries at this time. In some countries where it was not permitted, regulations were reviewed so that staple foods could be fortified so as to increase availability of folic acid in the food supply, at food manufacturers' discretion (10).
There was public, professional, and political debate in many countries during the mid-1990s about how best to respond to the epidemiological evidence for the folic acid- neural tube defect relationship. Although some initially questioned the quality of the evidence, most of the debate focused on what was the preferred policy response.
Complicating the debate in several countries was its intertwining with another vexed food policy debate – the use of health claims on food labels and in food marketing, which were prohibited at that time (11). Health claims identify a relationship between a food or a food property and a health effect, such as 'food product X can help reduce the risk of heart disease'. The use of health claims equates foods with therapeutics, identifying them as having 'functional' qualities, as health-giving or protective against disease. In 1995 the Kellogg Company, and the March of Dimes (which has the mission 'to improve the health of babies by preventing birth defects, infant mortality, and premature birth') (11) jointly developed a folic acid health message for placement (12).
A related development in Australia in 1998 involved the health minister speaking at a Kellogg's 'Nutrition Summit'. He referred to the need to review the existing prohibition on health claims in that country, and said that the folic acid-neural tube defect health message needed to be communicated (13). Subsequently a folic acid-neural tube defect health claim, linking consumption of the fortified food product with a reduced risk of defects, was devised (14). This health claim was established as a pilot project, creating the exception to the existing prohibition on health claims in Australia.
The appeal to food manufacturers was that it opened the door slightly on the existing prohibition of health claims. The appeal to food regulators was that an increased amount of folic acid would be available in the food supply. In 1996 Oman became the first country to implement mandatory fortification when it approved the addition of 5 milligrams per kilogram of folic acid to white flour (15). In the same year the US Food and Drink Administration issued regulations requiring that all 'enriched' cereal grain products be fortified at 140 micrograms per 100 grams cereal grain by 1 January 1998 (16).
The 2000s
The impetus that the US regulations created gave momentum for this policy option to be considered in many other countries, and they provided a template for technical considerations such as what would be the appropriate level of folic acid fortification. Since then, national policies for mandatory fortification have been agreed and put in place throughout Latin America, the Middle East, and parts of Africa and the Western Pacific.
In 2004 a consortium composed of the Flour Fortification Initiative (see below), the Centers for Disease Control and Prevention, and the Mexican Institute of Public Health, jointly convened in Cuernavaca, Mexico a technical workshop on 'Wheat Flour Fortification: Current Knowledge and Practical Applications' (17). The workshop was also supported by the March of Dimes, the Global Alliance for Improved Nutrition (GAIN), and the Micronutrient Initiative (see below).
In 2008 the Flour Fortification Initiative hosted its second technical workshop, this time on 'Wheat Flour Fortification: Practical Recommendations for National Application' in Georgia, USA, to provide advice for countries considering national wheat or corn (maize) flour fortification (18). The papers presented at the workshop endorsed mandatory fortification as well as other food fortification policies. The steering committee for this workshop consisted of representatives of the supporters of the workshops, including from the World Health Organization.
The following year WHO issued a consensus statement endorsing fortification of flour with folic acid, and also iron, vitamin B12, vitamin A, and zinc (19). These guidelines, developed from the 2008 workshop, were prepared by the core group from WHO, in partnership with the UN Food and Agriculture Organization, the UN Children's Fund, and the other supporters.
The 2010s
In 2010 a special supplement of the Food and Nutrition Bulletin, 'Flour fortification with iron, folic acid, vitamin B12, vitamin A, and zinc: Proceedings of the Second Technical Workshop on Wheat Flour Fortification' (20) was published. It also drew from the 2008 workshop. It repeated the call for mandatory fortification. In 2010, the WHO World Health Assembly and its Executive Board adopted a number of resolutions and decisions in relation to birth defects (21). Member states were urged to increase coverage of folic acid supplementation. The WHO director-general was requested to support member states in developing national plans for implementation of food fortification strategies, for the prevention of birth defects and to promote equitable access to such services.
As at 2012, 66 countries have instituted or agreed mandatory fortification of flour with folic acid as national policy, mostly in wheat flour and within the range 100–300 micrograms per 100 grams (22). The primary motivation has been neural tube defect prevention, or else as a conventional food fortification policy responding to evidence of population-wide folate deficiency. Three countries (Ireland, New Zealand, UK) initially did recommend mandatory fortification but subsequently deferred their recommendation. At the time of writing the US is reviewing its policy to consider increasing the number of food products mandated to be fortified with folic acid.
Benefits, risks, ethics
Mandatory fortification has benefits and risks. It is effective in helping prevent neural tube defects, though the level of effectiveness depends on baseline prevalence and folate status of the target group. It is equitable in that it passively increases the folic acid intake of everyone who consumes products made from fortified flour. Its key practical advantage in achieving effectiveness and equity, that it passively exposes the target group to increased folic acid, is also its key disadvantage, in that it indiscriminately exposes everyone in the population to novel levels of a synthetic vitamin for the rest of their lives.
The indiscriminate nature of mandatory fortification exposes this policy option to concerns about its public health risks. Its action in increasing the population's folic acid intake has been described as a form of 'uncontrolled clinical trial' (23), and as a 'double-edged sword' (24).
The ethical justification for mandatory fortification is weak. It is not proportional at the population level, it is not necessary, it has a high level of infringement, and rarely has been publicly justified. Relative to alternative policy options, mandatory fortification has more public health benefits except for preventing recurrent defects. In these cases supplementation is the most effective and equitable policy, as the necessary 4-5 milligram dose, ten times or more higher than obtained from fortification, could be made available, and intended recipients would be aware of the need of it.
Alternative policy options have not been evaluated to the same extent as mandatory fortification for their effectiveness and cost-effectiveness. The ethical justification for alternative policies, which are voluntary fortification or supplementation, or nutrition education or making no changes, is stronger than for mandatory fortification.
It is critical to match a potential policy option to the underlying cause of a policy problem. The degree of alignment of a potential policy option with the underlying cause of neural tube defects is predictability of the extent of public health benefit and risk, and ethical considerations. Supplementation is the policy option most directly responsive to the evidence of causation.
The second lesson is the importance of local circumstances in influencing the case for the different policy options. Countries with relatively high neural tube defect rates, low folate status (especially if associated with anaemia) and a high proportion of unplanned pregnancies, are likely to achieve a higher reduction in neural tube defect prevalence (and anaemia prevention) from mandatory fortification. This is by contrast with countries that have a relatively low defects rate, high folate status and low proportion of unplanned pregnancies. Differential impacts should guide assessment of public health benefits and risks, and ethical considerations, associated with each policy option for any particular country.
A political issue

Mandatory fortification of flour with folic acid is in place in the countries shown in blue in the map above. Coverage of Africa (right) is mostly voluntary
Policy-makers in countries around the world interpret the evidence in different ways as they formulate different policy responses. This is a highly contested and controversial public health policy topic. There are geographical clusters of countries that have recommended mandatory fortification. These as shown above, include the Americas, the Middle East, parts of Africa, and the Western Pacific. There are other geographical clusters where mandatory fortification has not been recommended, most notably Europe where a diversity of voluntarily fortified foods are available and promotion campaigns have been implemented, albeit usually on a short-term basis.
Few policy-makers question the epidemiological evidence for the folic acid-neural tube defect relationship. The debate is political, and is ostensibly about which policy option is best supported by the evidence. There are many actors within countries and globally that are involved in activities to promote mandatory fortification. A brief description of the role and influence of the more prominent global actors follows.
The actors
The actors listed here all work together to promote the mandatory fortification of flour with folic acid.
US Centers for Disease Control and Prevention (CDC)
In 1992 CDC recommended that all women of childbearing age consume 400 micrograms of folic acid daily to help prevent neural tube defects (9). Around this time, its then director of its division of birth defects and developmental disabilities, Godfrey Oakley, along with the March of Dimes, began advocating that folic acid to be added to the US standard for enriched flour (25). CDC continues to be highly supportive of mandatory fortification, describing it as one of the ten great public health achievements in the US during the decade 2001-2010 (26). Now CDC has developed a 'Global Initiative to Eliminate Folic Acid-Preventable Neural Tube Defects'. The aim is to increase the number of low- and middle-income countries that use mandatory folic acid fortification of 'high penetrance staples'. Among its strategic objectives are to work with WHO and others 'to establish a global policy to support and advance country-level fortification efforts (27).
CDC has nurtured many of the prominent global actors. In 2004 it supported the formation of the Flour Fortification Initiative (see below) (28) which it still supports strongly, and it continues to fund FFI's global secretariat. Godfrey Oakley has gone on to become one of the strongest advocates for mandatory fortification, as has the head of WHO's micronutrient unit Juan Pablo Pena-Rosas, who previously worked at CDC monitoring and evaluating flour fortification programmes (29).
Flour Fortification Initiative (FFI)
FFI is the world's leading advocate for mandatory fortification. Formed in 2004, it is a public-private partnership, a network of organisations working towards making fortification of wheat flour a standard practice globally. Its goal is for '80% of the world's roller miller flour to be fortified with at least iron or folic acid by 2015' (18). It has a well-developed and resourced strategy to work with national leaders to advocate flour fortification, and to provide technical assistance and resources for putting fortification plans into practice. It has placed mandatory fortification of flour with folic acid on the political agenda internationally.
Micronutrient Initiative (MI)
MI is a public-private partnership. Its motto is 'solutions for hidden hunger'. It supports folic acid mandatory fortification and also supplementation, especially in Bangladesh, India and Nepal (30). In 2003 it was the prime mover in establishing a coalition of international organisations to advocate worldwide action to increase folic acid consumption (31).
Global Alliance for Improved Nutrition (GAIN)
GAIN's goal is to reach 1.5 billion people with fortified foods including foods fortified with folic acid (32). GAIN is public-private partnership and is a powerful organisation. It is funded with sums up to or around $US 100 million yearly by the Gates Foundation, and is also supported by the US Agency for International Development.
World Health Organization (WHO)
WHO support for MFFFA is strong, as shown in its 2009 recommendations on wheat and maize flour fortification (6). The WHO receives grants from MI, CDC and GAIN for this programme, and is actively engaged in partnerships with these organizations as well as FFI. As noted, the head of the WHO micronutrients unit, Juan Pablo Pena-Rosas, previously worked at CDC. In 2011 he was appointed an adjunct assistant professor at the Rollins School of Public Health at Emory University, where Dr Godfrey Oakley is based and where the FFI website is hosted.
Their agenda
All these actors are influential and well-resourced advocates for mandatory fortification of flour with folic acid as the preferred policy option to help prevent neural tube defects. There are no equivalent well-organised actors that advocate for alternative policy options. There is some 'push-back' questioning mandatory fortification in the scientific press, especially from work in Europe, but this does not have the same impact. The actors above present a united front, complementing each other's activities, participating in a network of interactions as an effective coalition.
Global health governance
The global health governance agenda generated by public-private partnerships has enabled certain actors to gain privileged access to the UN system and to participate in key policy-making developments, including to promote mandatory fortification. WHO's own involvement as a public partner includes engagement with CDC, FFI, MI and GAIN, in policy discussions that preceded and then included its 2009 recommendations on wheat and corn (maize) flour fortification (6). The WHO micronutrients unit receives grants from MI, CDC, and GAIN, among others. WHO policy is that donors do not fund specific guidelines and do not participate in any decision related to the guideline development process.
International food trade
International food trade has not been an explicit influence on mandatory fortification policy. An exception followed the US decision to go for mandatory fortification. Originally Canadian food regulators did not support this, and they urged the US FDA not to proceed. However, Canadian flour millers were not prepared to produce different flours for the domestic and US markets, and applied the political pressure that led Health Canada to recommend mandatory fortification for Canada (33).
The medical model
In their analysis of the policy debate in Australia and New Zealand, two scholars conclude that a biomedical frame of reference dominates how mandatory fortification is represented in the media and professional journals. They comment that this observation reflects the traditional power and influence of the medical profession, in framing the debate, influencing the policy process, and shaping the ultimate decision for mandatory fortification (34).
The dominant role of the medical profession in shaping public health policy has been understood for many years (35). What is unusual here is that exertion of medical influence is in a reverse orientation from that normally observed. Rather than advocacy focusing on the use of a medical intervention to help solve a public health problem, as occurs when a nutrient supplement is proposed to correct a population-wide nutrient deficiency, here a public health intervention is being appropriated to help solve a medical problem.
Thus the policy-making process associated with the mandatory fortification of flour with folic acid internationally combines an advocacy coalition framework and a network approach. When policy options have been recommended, a strong predictor of mandatory fortification has been the combination of actors, activities and agendas working in concert. Powerful actors with a shared belief in mandatory fortification have operated both independently and as part of a coalition of actors. They have been dominant. There has been no alternative coalition with different beliefs. Those who believe in alternatives operate more as individuals. The coalition has undertaken sophisticated and persistent advocacy to influence key events and policy outcomes.
The way that evidence of benefits and risks of policy interventions to decrease neural tube defect prevalence has been framed, explains how scientific uncertainties and ethical dilemmas have been rationalised. The global health governance agenda that now encourages and even seeks out public-private partnerships, has amplified the influence of these advocacy coalitions by facilitating their access to United Nations agencies and key policy-making forums.
Supplementation

Folate, as its name implies, is in many leafy vegetables and other plant foods, and also in whole grains. Many food products are now fortified with folic acid
Advocacy for mandatory fortification can be compelling for governments wanting to be seen to be acting. It is a relatively straightforward policy that can achieve demonstrable change in population folate status relatively quickly. Alternative policy options such as supplementation require more sophisticated approaches and a sustained investment to achieve similar changes and outcomes.
Supplementation (not fortification) was used in the original clinical trials starting in the late 1970s and continuing to the early 1990s, that produced convincing evidence that folic acid reduces the risk of neural tube defects. In future there is a strong case for supplementation as the preferred policy option. It most closely aligns with the cause of neural tube defects. It has the potential for the greatest reduction in their prevalence. It has a low level of public health risk. It is ethically justified.
The primary constraint is political will. Many governments have stated a commitment to neural tube defect prevention. But they have rarely matched such statements with sufficient and sustained investment in folic acid supplementation to enable it to achieve its full potential (36,37).
Box 2
Folate in food
Editor's note. Mark Lawrence's book is about food fortification. In it he discusses the benefits and risks of mandatory as distinct from voluntary foritification, and also supplementation (see Box 1). He also mentions as further options, public information and education campaigns, and 'the status quo' – doing nothing.
There is a further option, beyond the remit of the book, which is to improve food systems and supplies so that they are much better sources of folate. Since the 1970s, when the nature, presence and properties of folate had become well understood, commentators have pointed out (2) that diets that are low in fresh foods and whole grains are poor sources of folate, which is found mostly in fresh or whole plant foods. Pioneering epidemiological work in the UK showed an impressive correlation of high prevalence of neural tube defects with low consumption of folate, and a multi-centre intervention trial showed impressive protection among women given supplements of folic acid (38). This and later bigger international trials (4,8) amounted to a body of work agreed to prove that folic acid supplementation – or fortification – protects against neural tube defects.
These studies have usually been interpreted as meaning that protection against neural tube defects must come from folic acid, and not from the folate in healthy diets. As a result, policy options are framed as either supplementation or fortification of food ingredients or products, or administration of pharmacological amounts of folic acid to women believed to be at high risk of having babies with neural tube defects. In the high politics of policy making meticulously presented by Mark Lawrence, the food option has got lost.
Conclusion
Mandatory fortification of flour with folic acid has created a precedent for mandating other versions of food fortification. So far it is the only example of food fortification being agreed and implemented, whose rationale is to add a nutrient to prevent disease in those at special risk, as distinct from than tackling population-wide nutrient shortage or deficiency. For this reason mandatory fortification is a complex and controversial policy option. The use of food fortification in this case is not without reason. There is as yet no way efficiently to target women who are predisposed to having a neural tube defect-affected pregnancy. In those countries where mandatory fortification is the policy option used, it generally prevents almost one-half of neural tube defect cases, usually in an equitable fashion.
Nevertheless, this novel use of food fortification in effect as a medical treatment, creates a precarious situation. The mandatory fortification of flour with folic acid is delivering a synthetic form of a vitamin in what accumulatively can be relatively high amounts to the target group, but indiscriminately, so that everyone who consumes the fortified foods will have an increased intake of folic acid. For infants, children, men and older adults, this raised folic acid intake will occur without apparent benefit and often without their knowledge.
The need to formulate public policy in a context of scientific uncertainties and complicating circumstances brings many political dynamics to the surface. In many of those countries where mandatory fortification has been adopted, a medical view of food and health relationships has dominated policy-making. A compelling combination of powerful actors have undertaken sophisticated advocacy and have been supported by the agendas now followed in global health governance.
More than twenty years after convincing epidemiological evidence that folic acid reduces the risk of neural tube defects was published, approximately one-third of countries around the world have adopted the mandatory fortification of flour with folic acid. Few governments have invested substantially and sustainably in alternative options. They could do so. For instance, folic acid supplementation involving primary health care delivery services are a promising option, with results that can compare with those of mandatory fortification and with less public health risk and no ethical considerations. There remain many unknowns. Whatever policy option is chosen, interventions must be monitored and evaluated, so as to refine and improve future practice.
References
- Wynn M, Wynn A. Prevention of Handicap and the Health of Women. London: Routledge and Kegan Paul, 1979.
- Darnton-Hill I, Mora J, Weinstein H, Wilbur S, Nalubola P. Iron and folate fortification in the Americas to prevent and control micronutrient malnutrition: an analysis. Nutrition Reviews 1999; 57(1):25–31.
- Christianson A. Howson C, Modell B. The March of Dimes Global Report on Birth Defects: The Hidden Toll of Dying and Disabled Children. New York: March of Dimes Birth Defects Foundation; 2006. Available at: http://www. marchofdimes.com/downloads/ Birth_Defects_Report-PF.pdf.
- Wald N. Folic acid and the prevention of neural tube defects. Annals of the New York Academy of Sciences 1993; 678:112–129.
- Rosenberg I. Folic acid fortification. Nutrition Reviews 1996; 54(3):94–5.
- World Health Organization. Recommendations on wheat and maize flour fortification meeting report: interim consensus statement, 2009..Available from: http://www.who.int/ nutrition/publications/micronutrients/wheat_ maize_fortification /en/index.html.
- Czeizel A, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. New England Journal of Medicine 1992; 327:1832–1835.
- Medical Research Council Vitamin Study Research Group. Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study. Lancet 1991 338:131–137.
- Centers for Disease Control and Prevention. Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. Morbidity and Mortality Weekly Report 1992; 41:1–7.
- National Health and Medical Research Council. NHMRC revised statement on the relationship between dietary folic acid and neural tube defects such as spina bifida. 1993..
- March of Dimes. History. Available from: http://www.marchofdimes. com/mission/history_qa.html.
- Anon. Kellogg and March of Dimes develop folate health message for product 19. Food Labeling News 22 June 1995.
- ANZFA. ANZFA Media News 18 March 1998.
- Australia New Zealand Food Authority. An interim code of practice for the communication of the health benefits of food products to be used in a pilot for health claims relating to folate/neural tube defects 1998–1999 was approved. Canberra: Australia New Zealand Food Authority, 1998.
- Alasfoor D, Elsayed M, Mohammed A. Spina bifida and birth outcome before and after fortification of flour with iron and folic acid in Oman. Eastern Mediterranean Health Journal 2010; 16(5):6.
- US Food and Drug Administration. Food standards: amendment of standards of identity for enriched grain products to require addition of folic acid. Federal Register 1996; 61(4):8781–8797.
- Flour Fortification Initiative. Report of the Workshop of Wheat Flour Fortification. Cuernavaca: Flour Fortification Initiative, 2004. Available from: http://www.sph.emory. edu/wheatflour/CKPAFF/index.htm.
- Flour Fortification Initiative. Available from: http://www.sph.emory.edu/ wheatflour/FortifyForLifeMedia.
- World Health Organization. Recommendations on wheat and maize flour fortification. Mmeeting report: consensus statement. 2009 [updated version].
- Serdula M, Peña-Rosas J, Maberly G, Parvanta I. Flour fortification with iron, folic acid, vitamin B12, vitamin A, and zinc. Proceedings of the Second Technical Workshop on Wheat Flour Fortification. Food and Nutrition Bulletin 2010; 31 (Suppl 1).
- World Health Assembly. Resolution WHA63.17. Birth defects. In: Sixty-third World Health Assembly, Geneva 17-21 May 2010. Resolutions and decisions. Geneva: World Health Organization; 2010.
- Lawrence M, Kripalani K. Profiling National Mandatory Folic Acid Fortification Policy Around the World. New York: Springer; 2012.
- Skeaff M, Green T, Mann J. Mandatory fortification of flour? Science, not miracles, should inform the decision. New Zealand Medical Journal 2003; 116(1168): U303.
- Lucock M, Yates Z. Folic acid fortification: a double-edged sword. Current Opinion in Clinical Nutrition and Metabolic Care 2009; 12(6): 555–564
- Flour Fortification Initiative. Fifteen years of fortifying with folic acid reduces birth defects; averts healthcare expenses. Available from: http://www.sph.emory.edu/wheatflour/FortifyForLifeBackground.pdf.
- CDC. Ten great public health achievements. United States, 2001-2010. Morbidity and Mortality Weekly Report 2011; 60(19):619–623. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a5.htm?s_ cid=mm6019a5_w.
- CDC. Global initiative to eliminate folic acid-preventable neural tube defects. Available from: http://www.cdc.gov/ncbddd/folicacid/global.html.
- CDC. CDC grand rounds: additional opportunities to prevent neural tube defects with folic acid fortification. Morbidity and Mortality Weekly Report 2010; 59(31):980–984. Available from: http://www.cdc.gov/mmwr/preview/ mmwrhtml/ mm5931a2.htm.
- Pena-Rosas JP, Parvanta I, van der Haar F, Chapel TJ. Monitoring and evaluation in flour fortification programs: design and implementation considerations. Nutrition Reviews 2008; 66(3):148–162.
- Micronutrient Initiative. Folic acid. Available from: http://www. micronutrient.org /English/View.asp?x=581.
- Oakley G, Bell K, Weber M. Recommendations for accelerating global action to prevent folic acid-preventable birth defects and other folate-deficiency diseases: meeting of experts on preventing folic acid-preventable neural tube defects. Birth Defects Research Part A: Clinical and Molecular Teratology 2004; 70(11):835–837
- Global Alliance for Improved Nutrition. About GAIN. 2011. Available from: http://www.gainhealth.org/about-gain
- Oakley GP. Folate deficiency is an 'imminent health hazard' causing a worldwide birth defects epidemic. Birth Defects Research Part A: Clinical and Molecular Teratology 2003; 67(11):903-904.
- Begley A, Coveney J. Wonder vitamin or mass medication? Media and academic representation of folate fortification as a policy problem in Australia and New Zealand. Australian and New Zealand Journal of Public Health 2010; 34(5):466-471.
- Illich I. Limits to Medicine: Medical Nemesis: the Expropriation of Health. New York: Penguin; 1977.
- Rofail D, Colligs A, Abetz L, Lindemann M, Maguire L. Factors contributing to the success of folic acid public health campaigns. Journal of Public Health (Oxford) 2012; 34(1):90–99.
- Al-Wassia H, Shah P. Folic acid supplementation for the prevention of neural tubedefects: promotion and use. Dovepress 2010, 2:105–116.
- Smithells R, Sheppard S, Schorah C et al. Possible prevention of neural tube defects by periconceptual vitamin supplementation. Lancet 1980, I, 339-340.
Acknowledgement and request
Extracted and digested from Lawrence M. Case study 2: mandatory flour fortification with folic acid. [Chapter 6]. In: Food Fortification. The Evidence, Ethics and Politics of Adding Nutruients to Food. Oxford: Oxford University Press, 2013.
Conflicting or competing interests: none declared.
Readers may make use of the material in this commentary if acknowledgement is given to the Association, and WN is cited. Please cite as: Lawrence M. Fortification. Folic acid and spina bifida. Is it safe? Is it wise? Is it right? World Nutrition March 2013, 4, 3, 95-111. Obtainable at www.wphna.org.
All contributions to World Nutrition are the responsibility of their authors. They should not be taken to be the view or policy of the World Public Health Nutrition Association (the Association) or of any of its affiliated or associated bodies, unless this is explicitly stated.