World Nutrition
Volume 3, Number 2, February 2012
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary.
Empowering our profession
Access pdf of this commentary here
Access pdf of commentary on WN here

Roger Hughes
School of Public Health, Bond University, Gold Coast, Australia
Email: roger_hughes@bond.edu.au
Roger Shrimpton
Independent consultant, Olhão, Portugal
Elisabetta Recine
Department of Nutrition, University of Brasília, Brazil
Barrie Margetts
Public Health Nutrition, Faculty of Medicine, University of Southampton, UK
Introduction
This commentary provides a rationale for codification of the competencies required for effective public health nutrition practice, and for providing the architecture for public health nutrition workforce development in the form of a competency framework. It is a prelude to the capacity building and professionalisation activities of the World Public Health Nutrition Association (the Association).
Public health nutrition has been a developing field of public health theory and practice for decades. However, it has only relatively recently been seen in the context of workforce development as a strategic component of building capacity for effective action. This focus, initially directed at under-nutrition, has more recently been applied as a gradual response to public health priorities such as non-communicable diseases (particularly cardiovascular disease) and more recently, obesity, diabetes and preventable cancers. This increase in focus in high-income countries, in response to the unsustainable burden of over-nutrition, has grown in parallel with a recognition that workforce capacity is a critical missing link in scaling up nutrition actions in order to accelerate the reduction of maternal and child under-nutrition in lower and middle income countries, many of which face the double burden of disease (1-3).
Workforce development is needed at a global level in order to create a workforce and a broader capacity that is central to achieving gains in population health in both higher- and lower-income countries. The development of the public health nutrition workforce, and a designated professional workforce tier, has been a priority capacity building initiative in a limited number of high-income countries (such as Australia, New Zealand, Canada and the US). In the main however, there is considerable diversity of workforce capacity, with most countries having under-developed workforces to address public health nutrition issues.
The emphasis on developing designated public health nutritionists as a workforce and professional group, distinct from clinically orientated dietetics or medical nutrition workforce models, recognises that population-based and promotional-preventive actions are required to address malnutrition in both forms. This requires different work that complements clinical practice and consequently requires additional competencies, the knowledge, skills and attitudes to perform this work (4).
Competencies and capacity
The capacity of the public health workforce is a key contributor to the ability of communities to address public health nutrition issues (5). Workforce capacity is influenced by a range of determinants including the quality of workforce preparation and continuing professional development, workforce size, organisation, and support (6). With respect to workforce preparation and continuing professional development, competency-based approaches have been widely embraced as a process central to the professionalisation of public health and its related disciplinary groups (7-11), including public health nutrition (11).
In the international context, workforce development that encourages optimal workforce mobility and collaboration in research and practice requires the development of comparably competent practitioners who are capable of developing and undertaking effective population-based strategies and practice to meet nutrition and public health objectives. This has been the position of workforce development scholars for at least the last decade (12-13).
Box 1
Competency standards
Competency standards provide the architecture for workforce development by codifying the knowledge, skills and attitudes (ways of thinking) necessary to effectively practice public health nutrition (14).
They have a deliberate focus on effective performance in the workplace, ensuring that workforce preparation and continuing professional development not only enhances what practitioners know, but also that they know how, can show how, and do' (15,16).
The competences movement
Competencies, competency standards and credentialing are all variations on a world-wide movement within the education, training and professional sectors. Competency based-training has been embraced by government and industry in many countries as a result of the economic rationalistic drive for efficiency since the 1980's. This movement is based on the premise that people need to be taught knowledge, skills and attitudes required in the workforce and that these are observable and assessable. This is supported by an argument that competency-based training would enhance the education sector's responsiveness to the economy and produce reliable outcomes (17,18).Competency standards are defining statements about a profession or work role that can be used to assist credentialing. Credentialing is the establishment of a self-regulatory process instituted by the relevant profession to determine and acknowledge that an individual has demonstrated competence to practice (18).
There is now a considerable literature debating the merits and limitations of the competencies movement (18-23). This debate has been mostly related to the broader training and education environment rather than specifically applied to nutrition or public health, but it is worth considering in any deliberation about the value of competency development for public health nutrition. Differences in the theoretical and philosophical underpinnings of the competencies movement have been the basis for this disagreement and debate.
The behaviouralist approach has its origins in the efficiency movement (24). It sees competency as the ability to complete discrete behaviours. This conception tends to atomise tasks, making them easier to measure, but makes training and assessment task focused, which is reductionist rather than holistic. A preoccupation with tasks ignores underlying attributes such as the ability to make judgements and perform multiple tasks simultaneously, overlooking the complexity of performance in the real world. By contrast, the holistic or integrated approach draws from the progressive education movement (24) and is concerned with teaching attributes such as critical thinking under the assumption that they will be applied in the workplace in specific contexts. This view is concerned with the way knowledge, attitudes, values and skills are used in combination, in particular situations. In this perspective, competencies are relational, involve reflective practice and place importance on context (18).
Competency-based training has aroused much controversy, especially among educationalists with a commitment to preparing people as citizens in society rather than just for the workforce, who argue that an overemphasis on competencies can mean that people only become skilled in relation to a particular occupation (25). Advocates of the competency-based training approach see it as a countervailing force against education producing people who know but cannot do (25).
A summary of the arguments in favour and against competency-based training is provided in Table 1, which should be considered when applying competency standards in a workforce development context. Given these arguments, a holistic or integrated view of competencies is being applied to this competency framework.
Right from the start, one of the forces that motivated Association members, has been the vision of public health nutrition becoming a more influential force for good in the world, and particularly in less resourced continents and countries. This argued for an electronic journal with – at least at first – unlimited access including to the whole website, and to pdfs of contributions.
Table 1
Arguments for and against competency-based training
| Arguments for |
|
| Role clarity, delineation | Competency standards aim to define the work and performance of the profession and therefore help define and delineate roles. Preventing overlap between professions may improve efficiency and this has been a compelling argument in favour of competencies. |
| Accountability, credibility | Standards help define the nature of the work of a profession and help communicate the complexity of work which may increase the credibility of the profession amongst the community. |
| Education | Competencies provide clearer goals for educators, learners and assist with curriculum design and assessment |
| Consistency | Competencies can assist universities to produce graduates with consistent minimum competencies because they provide a common ground for discussion between teachers and the profession. |
| Equity | Competency measurement can increase equality between people from different backgrounds. i.e. assessed based on ability to perform rather than academic path or course completed. |
| Cross profession movement | The common language of competencies that are consistent between professions can enable transfer across disciplines or recognition in different countries. |
| Arguments against |
|
| Reductionism | The tendency of competencies and competency assessment to isolate components of performance ignores the complexity of work. |
| Efficiency is not effectiveness | A more competent worker does not necessarily lead to a more effective worker |
| Control and sameness | Competencies and the use of competencies as a basis of credentialing can constrain workforce construction and behaviour leading to lack of innovation and diversity |
| Checklists | Competency assessment can become complicated leading to a simplistic use of competencies as checklists. Skills performance without knowledge and context can be life-threatening in the health sector. |
| Towards mediocrity | Competencies prescribe minimum standards that might discourage excellence by reducing everything to the lowest common denominator. |
| Teaching to the test | Competencies may encourage a belief that if something is not measurable as a competency it is not worth doing or learning and threatens learning processes. |
| Questionable reliability | There is no evidence to support compryrmvy-based training as a reliable measure. |
| Reduced liberal education | The tendency of competencies to be reductionist may reduce elements of liberal education such as experimentation, and attributes like learning how to learn and problem solving. |
( From 18-23, 25)
Competency standards
Competency standards serve a number of workforce development functions. (See Box 2).These include providing a structure for the design and evaluation of curriculum that promote minimum standards, the assessment of individuals in terms of fitness to practice, direct continuing professional development and assist job evaluation and design.
Box 2
Functions of competency standards
Competencies serve an overarching function of providing the architecture for workforce development by codifying the knowledge, skills and attitudes necessary to effectively practice or work (perform) in the field. These provide a structure for:
- Curriculum design and evaluation. By ensuring competency development through teaching and learning corresponds with agreed competency needs
- Credentialing. By providing standards that can be used as benchmarks for practitioner recognition or registration (26).
- Performance review. By providing standards which enable employers and practitioners to review practises and development needs.
- Recruitment. By providing a framework for articulating the competency and qualification expectations in position descriptions (duty statements, selection criteria) (27).
- Career planning. By providing direction for individual practitioners' considerations about further development needs.
The utility of competency standards as a tool for workforce development is increasingly being recognised worldwide. Competencies specific to public health nutrition have been of interest to workforce developers in the US for at least three decades (28-30). In Australia, advanced-level competencies have been proposed to help delineate the roles and workforce development needs required for this developing workforce (11), and competencies have been codified as a basis for public health nutritionist registration (31). Recent workforce development scholarship in Canada has also focused on identifying the competency requirements needed by public health nutritionists (32). The UK Nutrition Society has developed a system for registration of public health nutrition practitioners as a public protection and quality assurance measure (26, 33), and this has included consideration of competency issues (33).
Needed: A competency framework
Public health workforce development scholarship over the last few years has emphasised the importance of developing a competent public health workforce as a precursor to increasing societal capacity to protect and promote public health (34-38). As a result, there has been an emphasis on developing competency standards to provide the architecture for workforce development in public health (39-41), preventive medicine (42, 43), health promotion (44,45), and health education (46). It has also been of interest to public health nutrition scholars internationally (47-51). In some high-income countries (Australia, Canada, UK), competency frameworks have been developed for the public health workforce. Many of the competencies identified in this literature (11-28, 52) are similar, with considerable overlap across disciplines. It is recognised that this analysis is limited to English-language literature and that there may be other examples in non-anglophone countries.
Public health nutrition is a specialisation within public health practice and will share many of the competencies identified as being core to public health practice. Despite this, reliance exclusively on broader public health competency frameworks, without consideration of the additional or specialty competency elements required for effective public health nutrition practice, is problematic. There are a number of arguments (53) for a specific competency framework to inform public health nutrition workforce development. These include:
- A tendency towards generalising the public health workforce is counterproductive to developing workforce effectiveness (54).
- Training and experience in nutrition science, food and nutrition systems knowledge and analysis is critical to effective practice in public health nutrition (55).
- Without specific articulation of public health nutrition competencies required, workforce development will be inefficient (56).
Understanding what's required
It has been argued previously that workforce development specific to public health nutrition should be directed by analysis of public health nutrition problems, prioritisation of work effort based on intelligence about the most effective interventions, and consideration of the essential work required effectively to intervene (60). This logic suggests that a clear understanding of the work required is a critical pre-requisite for effective workforce development. Functional analysis is a common analytical approach used to determine required worker competencies across many vocational and professional groups.
Various attempts have been made to identify the work needed from the broader public health workforce as reflected by core functions or essential services (35, 61, 62). The nomenclature used in these efforts has varied. The World Health Organization (WHO) and US scholars have codified 'essential' public health functions using different methods and meaning different things. WHO use the term 'essential' to indicate functions (minimum standards) which ensure that the public health system has the capacity to respond to emerging and priority needs, proceeding from concerns about rapid changes to health systems around the world. The US definition of 'essential' refers to practices that must be undertaken to ensure that public health functions are being performed (63). In Australia 'core functions' for public health have been developed differentiated by reference to established or emerging practice. In this work, core functions were defined as those being absolutely necessary, the absence of which would imply gaps in public health capacity (63).
Comparison of this core functions work between countries indicates considerable similarity in statements about the work needed by the public health workforce, such as monitoring and surveillance, intervention management (needs assessment, planning, implementation, evaluation), policy and legislative measures and public health service delivery. Public health core functions have obvious currency when considering public health nutrition workforce functions and the work these imply (53).
It is however unclear whether broad public health functions adequately describe the work needed from the public health nutrition workforce in a way that meaningfully assists workforce development specifically to address public health nutrition issues and challenges. Earlier public health nutrition workforce development research suggests that it is important to delineate specific functions for public health nutrition, and that a blanket application of public health function statements is inadequate for the purpose of workforce development (54, 64). One of the challenges therefore, is to identify the specific functions or work required of the public health nutrition workforce to inform workforce development initiatives.
Earlier attempts to codify core functions for public health nutrition have been developed to describe the work required of the public health nutrition workforce (65). In this case the proposed core functions for public health nutrition where underpinned by a number of relevant assumptions, including:
- Public health nutrition functions are defined as those activities (processes, practices, services and programs) undertaken by the workforce in order to promote optimal nutrition, health and well-being in populations.
- Core public health nutrition functions are those functions that are regarded as absolutely necessary, without which would imply gaps in public health capacity.
- The relative importance of functions may vary depending on the jurisdiction or workforce level.
- Core functions are inter-related and complementary.
- Core functions articulate the work required to effectively address public health nutrition problems or issues, and consequently provide a framework for identifying and conceptualising workforce development needs.
- Current public health nutrition work practices do not accurately align adequately with these core functions. They are therefore aspirational, outlining the practices required for effective public health nutrition action and are a pointer to practice improvement (65).
Table 2 sets out ten core public health nutrition functions derived from workforce development research in high-imcome countries (60, 66) that describe the nature of public health nutrition work.
Table 2
Ten core functions for public health nutrition practice

Core function: Those functions that are regarded as absolutely necessary, without which would imply gaps in public health capacity. Adapted from (60, 66).
The location of public health nutrition practitioners in the organisational structure of public health systems will vary considerably between countries. Table 3 gives examples from Brazil, Indonesia and Australia to demonstrate the contextual relevance of 'level of public health nutrition work'. Although the practice context will vary and the relative importance and or application of core functions will vary, there is a consistent pattern of work that defines public health nutrition practice (as broadly described by these core functions.
Table 3
Description of public health nutrition work
at different levels in the public health system
| Level descriptorsr |
Practice description |
| Local health service | The public health nutrition practitioner working at this level will have greater functions in building local community capacity, co-ordinating and value-adding to the nutrition-related work of non-nutritionist health and community workers via intervention management and the education of the public. They will usually have a relatively minor supporting role in monitoring and surveillance and research and analysis, but this can vary. |
| Province/regional health services | The public health nutrition practitioner at this level has a greater role in intervention management (provision of supplies, funding training of workforce, plus periodic supervision and monitoring), particularly in the development and roll-out of interventions across the provinces districts, usually includes coordination and support for district level teams. She/he has a greater monitoring and surveillance and research and evaluation function, and may coordinate provincial monitoring and surveillance. May have broader responsibility for service design and policy at Provincial level, as well as promoting inter-sectoral collaboration. Capacity building tends to focus on partnership building across sectors at provincial level, in addition to public health nutrition workforce development which may extend down to and facilitate at the district level. |
| State/ national | The public health nutrition practitioner at this level has major roles in development and evaluation of food and nutrition policy, managing departmental politics, may provide advice or direct resource allocation to provincial and district levels and works on a high level strategic planning. This level also includes the development and dissemination of norms and protocols for nutrition interventions at all levels. Usually has a major role in national or state food and nutrition monitoring and surveillance and coordinating research and evaluation activity. Capacity building tends to focus on resource allocation, leadership development, partnerships and to a lesser extent broader workforce development. |
Be it in Indonesia, Brazil, Australia or Mozambique (as examples), the relative importance of these ten core functions at different levels is probably very similar. Box 3 illustrates the relevance of these core functions in different practice contexts.
Box 3
Public health nutrition interventions
To control iron deficiency anaemia in a district could involve the following. The delivery of iron supplements to cure the anaemia of individuals, be it weekly in school children through school teachers, or daily in pregnant women through nurses, midwives and community health workers for extended outreach in antenatal care. The treatment of infections – presumptive malaria treatment during pregnancy and periodic de-worming for gastrointestinal tract worms in schools as well as in antenatal care. The distribution of insecticide treated bed nets. Promoting the use of shoes. Promoting the consumption of appropriate foods including those that are fortified (68). Anaemia is so common that these same approaches are likely to be applicable in many country settings.
Similarly to promote, develop and support healthy growth and development throughout all stages of the life-course requires focus on the period from conception to two years of age, as this is when growth faltering occurs and final adult height is largely determined.(69). This means ensuring that doctors, nurses and midwives properly treat and advise mothers during the 'continuum of care' (70) from conception to two years of age and from community through to central hospital. Tasks include ensuring that all infections are treated, and mothers are encouraged to eat properly, not to smoke. and to rest adequately in order to gain weight appropriately during pregnancy, as well as promoting exclusive breastfeeding during the first six months of life and adequate complementary feeding from six months onwards.
Nurses and midwives need training in the weighing and plotting of fetal and infant growth on appropriate weight and growth charts, including how to make these measurements properly and to counsel the mother accordingly. Most of these promotional activities are not aimed at sick individuals but at promoting health in the whole population, and so will depend on community based outreach to achieve high coverage. Indeed community participation has proven essential for most successful nutrition programmes (71).
In Indonesia, community participation is performed by village volunteers of the Family Nutrition Improvement Activities through the monthly village Posyandu meetings, and in Brazil by the community health workers of the Family Health Programme of the Ministry of Health. In Mozambique the coverage of the network of community health workers (Agente Polivalente Elementar) is still being expanded and the nutrition component of their activities yet to be fully developed. The real task for the district public health nutrition specialist is to have oversight and ensure high coverage of the package of interventions. If effectively targeted to mothers and children from conception to two years of age these could prevent at least a quarter of child deaths and reduce the prevalence of stunting by about a third (72).
What will be different by country are the need for the more curative nutrition interventions and those related to the treatment of other diseases, such as the treatment of severe acute malnutrition, which is very uncommon in Brazil now and getting much rarer in Indonesia, although still common in Mozambique, where increasingly it is associated with HIV/AIDS. In those countries with the double burden of disease or where chronic diseases are more common, such as Brazil, the public health services will increasingly need health workers to advise the public on safe and healthy food choices, as well as on dietary regimes for weight loss.
The capacity building function has to be one that occupies a lot of the time of the public health nutrition specialist at the district level, although very much supported by the provincial level specialist. The building of community capacity should take up most of the time at district level. Oversight of the capacity building function should be the one of the main parts of the work of the provincial level specialist. This will involve carrying out periodic supportive supervision as well as holding training provincial level training seminars and workshops for district specialists, as well as leading training workshops for other health professionals at the district level.
The research and analysis functions will increase in intensity and complexity going from the district to the centre. But the district level specialist still has considerable responsibility to keep a finger on the pulse, monitoring nutrition service delivery, and sending this intelligence upwards to the provincial specialist. The provincial specialist will aggregate this information and supplement it with other non-health service sources of information available at the provincial level and provide this on upward. At the national level this system level information will be supplemented with national survey information as well as evaluations. The national level specialist would have a major responsibility for evaluation of the effort of the workforce by developing either stand-alone evaluations, or incorporating appropriate data collection in other broader national surveys such as demographic and health surveys or household expenditure surveys (73).
Consensus on requirements
Attempts to assess consensus on the competency needs of public health nutritionists as distinct specialist practitioners in the early 2000s, demonstrated a high level of agreement on essential public health nutrition competencies. These were identified by an international panel of public health nutritionists from the US, Europe and Australia (74). Although panellists were recruited from a limited range of cultural and health system contexts, this finding supported the suggestion that competencies required for effective public health nutrition practice are largely consistent across countries and settings (at least in high-income countries) and that workforce development for public health nutrition can be based on a consensus set of competencies that are transferable across jurisdictions and in different contexts (14, 74). Many of the competencies identified were similar to those of general public health practice (7, 9-11), but with a consistent provision that the public health nutrition workforce requires additional competency units in nutritional sciences (74).
This earlier scholarship focusing on public health nutrition competencies has promoted a premise that the mix and level of competency required by an individual practitioner will vary in different practice contexts, but that there are a core set of essential competencies required for a practitioner to be assessed as competent (40). A similar study in 2008 (75) assessing consensus on competencies amongst an expert panel derived from European Union countries has reinforced these findings.
Participants from varying national practice contexts at the September 2010 Association capacity building workshop at the World Public Health Nutrition congress in Porto in 2009, considered this premise and agreed that the core competency requirements of a public health nutritionist are similar between higher and lower income countries.
Proposed framework
The competency framework for public health nutrition workforce development summarised below has been based on fusion of existing competency frameworks in the fields of public health in Australia (76), the United States (40) and the United Kingdom (39) and consensus developed via international Delphi studies (75, 77). It also cross-references to competency standards developed in the fields of health promotion (78) and advanced-level practice in dietetics (79).
Table 4 summarises the assumptions underpinning the competency framework described in this document.
Table 4
Description of public health nutrition work
at different levels in the public health system
|
*Preventive interventions may include primary, secondary and tertiary prevention. In many practice contexts, Public health nutritionists are treating under-nutrition at a population level (for example, micronutrient supplementation as a treatment for deficiency).
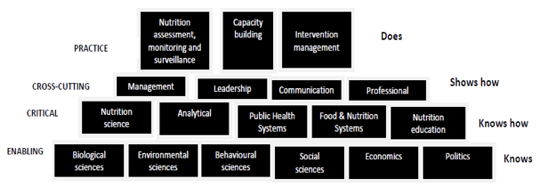
In this framework, the holistic-integrated approach to competency is applied, which outlines the complex combinations of attributes (knowledge, attitudes, ways of thinking, values, skills) required effectively to perform public health nutrition work as defined by public health nutrition core functions. Competence is conceived as a complex structuring of attributes needed for effective performance in specific or varied situations (22, 80). Figure 1 illustrates a framework delineating different competency modules that collectively describes the mix of these attributes required to effectively perform core public health nutrition work/ core functions. In this framework, different categories of competency units have been defined and positioned in different tiers of the building block framework. This organisation is informed by a number of principles relating to assessment and demonstration of competence informed by the Dreyfus model of skill acquisition (81-83) and hierarchies of competency assessment outlined by Miller (16).
These include:
- Enabling knowledge and skills are required that underpin higher order practice behaviours as the expression of competency.
- Critical competencies differentiate practice and help define specialisation of practice.
- Cross-cutting competencies exist that are common across professional public health and nutrition practice and help delineate professionalism.
- Practice competencies are higher order composite behaviours utilising a combination of knowledge, skills, values and attitudes to perform complex practice behaviours required to perform core functions.
Figure 1 depicts 18 clusters of competency units arranged as different layers or building blocks over four levels. In this model, higher level competency units/clusters (for example, practice competency level) involve a greater degree of behavioural performance (showing how and doing) than lower level and more cognitive competencies (knowing and knowing how).
Figure 1
Building blocks for effective public health nutrition practice
Work in progress
Public health nutrition practice is dynamic, influenced by the context of practice (such as location, workers level in the system, different problems) and changing over time. As a result, a static or rigid competency framework has less value as a guide to workforce development than a framework that adjusts to changes in needs, workforce practices and contexts.
To that end, the competency framework here, is a work in progress and should be viewed as a living document. To illustrate this point, a consensus development project (unpublished) utilising the Delphi technique has recently been completed in Australia to test the face validity of the competency framework among public health nutrition academics and practitioners from around the world. Preliminary analysis of this projects data suggests that as things are now, the framework is a good reflection of public health nutrition competency needs irrespective of country location and will help to fine-tune the framework over time. (See also 84-87).
This commentary invites readers to contribute to this process of enhancing the professional architecture we use to build workforce and overall capacity, by critiquing this framework, suggesting other competencies and applying this competency framework to local workforce development initiatives. Please use the response facility below, or send comments to the lead author. At the very least, it serves to illustrate the complexity of practice in public health nutrition, and reinforces the need for us all to be committed to life-long learning and professional development so that we stay at the forefront of our profession and effective in our practice.
References
- Gillespie S, McLachlan M, Shrimpton R, Combating malnutrition: Time to Act. World Bank-UNICEF Nutrition Assessment. 2003, World Bank: Washington DC.
- Heikens G et al., Nutrition interventions need improved operational capacity. The Lancet. 2008. 371 (9608): 181-182.
- Bryce J et al., Maternal and child undernutrition: effective action at national level. The Lancet., 2008. 371 (9611): 510-526.
- Hughes R, Somerset R, Definitions and conceptual frameworks for public health and community nutrition: a discussion paper. Australian Journal of Nutrition snd Dietetics 1997. 54(1): 40-45.
- Baillie E et al., A capacity building conceptual framework for public health nutrition practice. Public Health Nutrition, 2009. 12(8): 1031-1038.
- Hughes R., A socio-ecological analysis of the determinants of national public health nutrition workforce capacity: Australia as a case study. Family & Community Health 2006(29): 55-67.
- Council of Linkages. Core Competencies for Public Health Professionals 2009. http://www.phf.org/link/core-061109.htm
- Galway Consensus Conference (2008) Toward domains of core competency for building global capacity in health promotion: The Galway Consensus Conference Statement. http://www.sophe.org/upload/Galway%20Consensus%20Conference%20Statement%20-%20Final_84911642_6302008111733.pdf
- Health Scotland, Competencies for health promotion practitioners: Report of a working group. 2005, Health Scotland: Edinburgh.
- Public Health Agency of Canada, Core competencies for public health in Canada: Release 1.0, in www.phac-aspc.gc.ca/core_competencies 2007, Public Health Agency of Canada: Ottawa.
- Hughes R., A competency framework for public health nutrition workforce development. 2005, Australian Public Health Nutrition Academic Collaboration: www.aphnac.com
- Haughton B, Story M, Keir B. Profile of public health nutrition personnel: Challenges for population/system-focused roles and state-level monitoring. Journal of the American Dietetic Association 1998. 98(6): 664-670.
- Yngve A., et al., Effective promotion of healthy nutrition and physical activity in Europe requires skilled and competent people; European Master's Programme in Public Health Nutrition. Public Health Nutrition, 1999. 2(3a): 449-452.
- Hughes, R., Competencies for effective public health nutrition practice: a developing consensus. Public Health Nutr, 2004. 7(5): p. 683-91.
- Wass V., et al., Assessment of clinical competence The Lancet 2001. 357: 945-949.
- Miller G., The assessment of clinical skills/competence/performance. Academic Medicine, 1990. 65: S64-S69.
- Mayer C., Employment rel;ated key competencies; A proposal for consultation [The Mayer Report]. 1992: Melbourne.
- McAllister M. Competency standards: Clarifying the issues. Contemporary Nurse, 1998. 7(3): 131-137.
- Bowden J, Masters G Implications for higher education of a competenciy based approach to education and training. 1993, Department of Education and Training, Australian Government Publishing Service: Canberra.
- Chapman H. Some important limitations of competency-based education with respect to nurse education: An Australian perspective. Nurse Education Today, 1999. 19: 129-135.
- Hager P. Is there a cogent philosophical argument against competency standards? Australian Journal of Education, 1994. 38: 3-18.
- Gonzi A. Competency based assessment in the professions in Australia. Assessment in Education, 1994. 1: 27-44.
- Hager P, Gonzi A, Competency based standards: A boon for continuing professional education. Studies in Continuing Education, 1991. 13: 24-40.
- Preston B. Possibilities and implications of competency based standards for public health: In: System-wide learning for public health. 1995, Public Health Association of Australia: Canberra.
- Rivers K, Aggleton P, Whitty G, Professional preparation and development for health promotion: a review of the literature. Health Education Journal, 1998. 57: 254-262.
- Landman J. Training in public health nutrition: symposium at the 17th International Congress of Nutrition, Vienna. Public Health Nutrition, 2001. 4(6): 1301-1302.
- Hughes R. Employers expectations of core functions and competencies for the public health nutrition workforce. Nutrition and Dietetics, 2004.
- Sims L., Identification and evaluation of competencies of public health nutritionists. American Journal of Public Health, 1979. 69: 1099-1105.
- Story M., et al., Adolescent health and nutrition: A survey of perceived knowledge and skill competencies and training interests among dietitians working with youth. Journal of the American Dietetic Association 2000. 100(3): 362-364.
- Haughton, B, Story M, Keir B, Profile of public health nutrition personnel: challenges for population/system-focused roles and state-level monitoring. Journal of the American Dietetic Association 1998. 98(6): 664-70.
- NSA, Specialist competencies in nutrition science. 2007, Nutrition Society of Australia: Melbourne.
- Fox A. et al., Public health nutrition practice in Canada: a situational assessment. Public Health Nutrition, 2008. 11(8): 773-781.
- UKVRN, Professional registration in nutrition: Code of ethics and statement of professional conduct. 2007, The Nutrition Society. London.
- CDC/ATSDR. and CfDCAfTSaD. Registry., Strategic plan for public health workforce development. 2001, US Department of Health and Human Services.
- Kennedy V, Moore F, A systems approach to public health workforce development. Journal of Public Health Management Practice, 2001. 7(4): 17-22.
- Riddout L., et al., Planning framework for the public health workforce: Discussion paper. 2002, National Public Health Partnership: Melbourne.
- Gebbie K, Rosenstock L, Hernendez L. Who will keep the public health? Educating public health professionals for the 21st Century. 2002, Institute of Medicine National Academic Press: Washington DC.
- Lichtveld M., et al., Partnership for front-line success: A call for a national action agenda on workforce development. Journal of Public Health Management Practice, 2001. 7(4): 1-7.
- Healthwork UK, National standards for specialist practice in public health: An overview (Approved version). 2001, Healthwork UK: London. p. 7.
- Practice/HRSA, CoLbAaPH.Core competencies for public health professionals. 2002 [cited 2002 August].
- Genat B, Robinson P, Parker E, Foundation competencies for Master of Public Health graduates in Australia, ANAPHI, Editor. 2010, Australian Network of Academic Public Health Institutions: Melbourne.
- Lane D et al., Core competencies for preventative medicine residents: Version 2. American Journal of Preventive Medicine 1999. 16(4), 367-372.
- Medicine, ACoP. Core competencies and performance indicators for preventive medicine residents. 2002 [cited 2002 5.9.02].
- Precision Consultancy, Draft health promotion competency standards. 2000: Melbourne.
- Howat P et al., Development of competency-based University health promotion courses. Promotion & Education, 2000. VII(1): 33-38.
- NCHEC. Responsisbilities and competencies for health educators. 2002 [cited 2002 5.9.02]; Available from: www.nchec.org/competencies.htm.
- Nutrition Society, How to specify levels of learning outcome in public health nutrition; Annex. 2000, Nutrition Society: London.
- Dodds J, Polhamus B. Self-perceived competence in advanced public health nutritionists in the United States. Journal of the American Dietetic Association 1999. 99(7): 808-812.
- Landman J, Buttriss J, Margetts B, Curriculum design for professional development in public health nutrition in Britain. Public Health Nutrition, 1998. 1(1): 69-74.
- Pelletier D. Advanced training in food and nutrition: Disciplinary, interdisciplinary, and problem orientated approaches. Food and Nutrition Bulletin, 1997. 18(2): 34-145.
- Rogers B, Schlossman N. 'Public nutrition': the need for cross -disciplinary breadth in the education of applied nutrition professionals. Food and Nutrition Bulletin, 1997. 18(2): 120-133.
- Lloyd B., National Public Health Education Framework Project: Final Report. 2003, University of Sydney: Sydney.
- Hughes R. Public health nutrition workforce development: An intelligence based blue-print for Australia., in School of Health Science. 2003, Griffith University: Gold Coast.
- Hughes R. Public health nutrition workforce composition, core functions, competencies and capacity: Perspectives of advanced level practitioners in Australia. Public Health Nutrition, 2003. 6(6): 607-613.
- Hughes R. Competency development in public health nutrition: Reflections of advanced level practitioners in Australia. Nutrition and Dietetics, 2003. 60: 198-204.
- Hughes R. A socioecological analysis of the determinants of national public health nutrition work force capacity: Australia as a case study. Family and Community Health, 2006. 29(1): 55-67.
- Hughes R.. Competencies for effective public health nutrition practice: A developing consensus. Public Health Nutrition 2004.
- Campbell K. et al., Developing a public health nutrition workforce in Australia: Workforce issues. 1997, National Specialty Program in Public Health and Community Nutrition: Melbourne.
- Hughes R. Enumerating and profiling the Australian public health nutrition workforce. Nutrition and Dietetics, 2004.
- Hughes, R., A conceptual framework for intelligence-based public health nutrition workforce development. Public Health Nutrition, 2003. 6(6): 599-605.
- NPHP Public health practice in Australia today- Core Functions. 2001, National Public Health Partnership: Melbourne.
- Sapirie S. Essential public health functions. 1999 [cited 1999.
- Partnership, NPH. National Delphi study on public health functions in Australia. 2000, National Public Health Partnership: Victoria.
- Hughes R. Employers expectations of core functions and competencies for the public health nutrition workforce. Nutrition and Dietetics, 2004. 61: 105-111.
- Hughes R. Introduction to Public Health Nutrition Practice. In: Public Health Nutrition: From Principles to Practice. Worsley MLT (ed). 2007, Allen & Unwin: Crows Nest.
- Margetts B. Promoting the public health nutrition workforce in Europe. Final report of the Jobnut project. 2009, University of Southampton, UK.
- Hughes R. Competency development needs of the Australian public health nutrition workforce. Public Health Nutrition, 2003. 6(8): 839-847.
- WHO/UNICEF. 2004. Focusing on Anemia: Towards an integrated approach for effective anemia control. Geneva: World Health Organization
- Victora C, de Onis M, Hallal PC, Blössner M, Shrimpton R. 2010. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 125(3):e473-80.
- Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. 2007. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. The Lancet. 370(9595):1358-69.
- Shrimpton R, 1995. Community Participation in Food and Nutrition Programs: An Analysis of Governmental Experiences. In: Child Growth and Nutrition in Developing Countries, Pinstrup Andersen, P, Pelletier, D, Alderman, H. Cornell University Press. Ithaca NY
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev HP, Shekar M; Maternal and Child Undernutrition Study Group. 2008. What works? Interventions for maternal and child undernutrition and survival. The Lancet. 371(9610):417-440.
- Victora CG, Habicht JP, Bryce J. 2004. Evidence-based public health: moving beyond randomized trials. American Journal of Public Health. 94(3):400-405.
- Hughes R. Public health nutrition workforce composition, core functions, competencies and capacity: perspectives of advanced-level practitioners in Australia. Public Health Nutrition, 2003. 6(6): 607-613.
- Jonsdottir S et al., Consensus on the competencies required for public health nutrition workforce development in Europe - The JobNut project. Public Health Nutrition, 2010
- ANAPHI, National Public Health Education Framework Project: Final Report.Sydney:ANAPHI,2003. 2004: http://www.phlr.anaphi.unsw.edu.au/comp/comp.htm
- Hughes R. Competencies for effective public health nutrition practice: A developing consensus. Public Health Nutrition, 2004. 6: 839-847
- Shilton T et al., Review of competencies for Australian health promotion: Final report. 2002, Curtin University & National Heart Foundatation(WA): Perth
- DAA, Competency standards for advanced practice in dietetics. 2004, Dietitians Association of Australia: Canberra
- Grant G., Implications of competency-based education, in On competence: Critical analysis of competency based reforms in higher education., G. Grant, et al., Editors. 1974, Jossey-Bass: San Fransisco. 1-17.
- Dreyfus S, Dreyfus H. A five-stage model of the mental activities involved in directed skill acquisition. 1980, University of California: Berkeley
- Brenner P. Use of the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgement in nursing practice and education. Bulletin of Science Technology and Society, 2004. 24: 188-199.
- Crossley J, Humphries G, Jolly B. Assessing health professionals. Medical Education, 2002. 36, 800-804.
- PHAC, Core competencies for public health in Canada: Release 1.0. 2008, Public Health Agency of Canada: Ottawa.
- UKPHR. Application for defined specialist accreditation onto the UK public health register by retrospective portfolio assessment: Framework and guidance. 2006, United Kingdom Public Health Register.
- DAA, National competecy standards for entry-level dietitians in Australia. 2009, Dietitians Association of Australia: Canberra.
- Jonsdottir S, Measurement and development of European consensus on core competencies and curricula required for effective public health nutrition practice., in Department of Food Science. 2008, University of iceland: Rykjavik.
Acknowledgement and request
Readers are invited please to respond. Please use the response facility below. Readers may make use of the material in this editorial if acknowledgement is given to the Association, and WN is cited
Please cite as: Hughes R, Shrimpton R, Recine E, Margetts B. Empowering our profession.,[Commentary] World Nutrition, February 2012, 3, 2: 33-54. Obtainable at www.wphna.org
The opinions expressed in all contributions to the website of the World Public Health Nutrition Association (the Association) including its journal World Nutrition, are those of their authors. They should not be taken to be the view or policy of the Association, or of any of its affiliated or associated bodies, unless this is explicitly stated.
WN commentaries are subject to internal review by members of the editorial team.