World Nutrition
Volume 2, Number 8, September 2011
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
UN Summit on non-communicable diseases
Up to the Summit:
Inglorious paths


Philip James
International Association for the Study of Obesity
London School of Hygiene and Tropical Medicine
Email: jeanhjames@aol.com
Click here for member's profile
Click here for March report on WHO and the UN Summit
Click here for April report on DOHaD and the UN Summit
Click here for May report on NCD Alliance and the UN Summit
Click here for July report on civil society, industry, and the UN Summit
Click here for August report on UN Summit Political Declaration
Click here for this month's report on UN Summit crisis
Click here for editorial related to this commentary
Click here for associated short communications
Click here for pdf of this commentary here
Introduction
This month on 19-20 September, the General Assembly of the United Nations will hold its first High Level Meeting on the prevention and control of non-communicable diseases (also known as chronic diseases). While generally referred to – as here – as a summit, there is a difference. Formally, UN summits convene heads of state and government. UN high level meetings are usually held at senior ministerial level. This is a level below that at which the 2000 Millennium Development Goals, with their new time-based quantified targets, were agreed. Nor does it follow that a meeting on public health will be between ministers of health. Effective prevention and control of epidemic diseases involves finance, foreign affairs, industry and trade, whose ministers and representatives are likely to be present in force at the New York meeting this month.
A Political Declaration (1) of concern and commitment will be agreed and issued. (A draft of the Declaration is available as a pdf here). For all of us working in public health nutrition, and other public health fields, often for many years with relevant UN agencies, this might seem to represent a culmination of all our efforts. Instead, the climb has so far been on the whole a rather dispiriting journey. This commentary, together with the associated editorial and other contributions in WN this month, and elsewhere, gives some of the reasons why. My observations mostly derive from work in which I have myself been engaged with many colleagues over the last thirty or so years.
A change in mood
A reason to be gloomy is that in this century there has been a sea-change in circumstance and mood within the United Nations system, and in particular within the World Health Organization. The UN and its agencies have become increasingly starved of human and material resources, and in particular discretionary funds. At the same time, successive political and economic upheavals have led to stringent budget-cutting within relevant government departments even of wealthy UN member states. As a result, for practical reasons dressed as sound policy, powerful actors possessing huge amounts of discretionary funds have been invited or welcomed as partners in the formulation of global public policies. In our field these are the transnational food and drink processing corporations, together with the new philanthropies.
Up to and throughout the 1990s those industries whose products are harmful to health were usually and rightly kept at arm's length when policies designed to protect health were being formulated, although some would be invited to collaborate in the implementation and monitoring of programmes based on these policies. Now, such industries are increasingly being invited to participate in the creation as well as the implementation of policies and programmes, by the method known as 'public-private partnerships'.
Thus, in the draft Political Declaration as it developed from mid- to late July, the idea of a new 'Non-Communicable Prevention and Control Diseases Partnership' has been floated. This would 'guide actions and assess progress achieved in realizing voluntary commitments by all stakeholders in the prevention and control of NCDs'. The 'stakeholders' specified include 'international financial institutions' and 'the private sector' as well as UN member states, UN agencies, civil society organisations, foundations and research institutions. Experience so far shows that 'the private sector' includes and in practice overwhelmingly means the transnational food and drink processors and their representative and associated organisations. It may also include the alcohol industry or its associated organisations – an issue that needs to be confronted and addressed without delay.
This helps to explain a series of features in the documents so far released or discovered, prepared for this month's summit. In particular, recommendations on diet are expressed in general terms. But to be effective, policies on food, nutrition and the prevention and control of diet-related diseases have to include numbers – targets and goals that specify the composition of healthy diets, and that include quantified amounts for reduction for example of saturated fats, added sugars, and salt, such as those shown in Table 1. Throughout this century so far, and previously, numbers have constantly and successfully been opposed by the US, the biggest single funder of the United Nations, and by some other big UN players. So, targets do not appear in the latest documents being prepared for the summit. The chance of them appearing in its final Political Declaration is I think zero.
Being helpful to big business
Another and perhaps associated factor – which can be touched on only very briefly here – is that much of the most reliably attested evidence on diet, nutrition and non-communicable diseases has evidently been set aside by the very pressed secretariat responsible for preparations for the summit. Instead, remarkable reliance is being placed on other ideas which have rather a slender evidential basis. Curiously, other new evidence, which implies policies not in the immediate interests of the food and drink processors, has been overlooked. For example, studies show that children, now being bombarded with publicity for branded energy-dense fatty, sugary or salted products, are unable to make rational choices, because the brain is not fully mature until young adulthood. This has not been taken into account.
Analysis shows that in general, conclusions that are unhelpful to the food and drink processing industry are so far being downplayed, whereas conclusions that are consistent with or support the policies and bottom lines of these industries are being emphasised. Given the scale of the international food and drink manufacturing industry and its representative organisations, and their very strong presence in some of the formal and official processes preliminary to the NCD summit, this is hardly surprising. But such moves are flying in the face of reliably attested scientific evidence, and setting aside decades of careful independent policy recommendations and actions.
The established scientific findings
The ascent to the summit began on various long and winding paths, which have converged into one road in the last few years, months and weeks. The journey can be said to have begun back in the 1980s. At that time, compelling evidence had already emerged showing that the same group of dietary factors modified the risk of various chronic diseases, including those that are leading causes of disability and mortality. This led to the conclusion that policies to prevent and control these diseases should include recommendations and actions designed to maintain healthy dietary patterns and to change unhealthy ones.
The UN reports of 1990 and 2003
This was an important finding of the WHO '797'report published in 1990, the work of a WHO expert technical study group of which I was chairman (2). The conditions and diseases we specified included dental caries, obesity, diabetes (type 1), osteoporosis, cardiovascular diseases (coronary heart disease, and high blood pressure and cerebrovascular disease), a number of common cancers, non-cancerous conditions of the colon, and liver diseases. The report also took physical activity into account. Importantly, it also emphasised deficiency diseases. This month's summit, in discussing food and nutrition policies to prevent non-communicable diseases, needs to take into account that such policies, when enacted, also need to reduce childhood malnutrition and nutritional deficiencies.
This approach and these findings were essentially confirmed and strengthened by the further '916' report with the same theme, a joint initiative of WHO and FAO, published in 2003 (3). This was the work of an expert technical consultation chaired by Ricardo Uauy. In the intervening years the strength of evidence from consistent results of high-powered epidemiological studies and experimental investigations had greatly increased. The conditions and diseases examined by the '916' report were dental diseases, obesity, diabetes (type 2), osteoporosis, cardiovascular diseases; and also cancers, where the evidence had become remarkably stronger. Some of the quantified recommendations of the '916' report are shown in Table 1. These and others, derived from the evidence of studies accumulated since the time of the '797' report, and also going back to the 1970s, have been adopted by national governments all over the world, especially in the South, and suitably adapted to suit the needs of particular countries.
Table 1
Diet, Nutrition, and the Prevention of Chronic Diseases
The WHO '916' report issued in 2003 (3)
Some of its recommendations relating to the proposed
average intakes of populations needed to improve health
| % energy | grams/day | |
|---|---|---|
| Total fat | 15-30 | |
| Polyunsaturated fatty acids | ‹ 6-10 | |
| Saturated fatty acids | ‹ 10 | |
| Trans fatty acids | ‹ 1 | |
| Free sugars | ‹ 10 | |
| Salt | ‹ 5 | |
| Fruits and vegetables | ≥ 400 |
Three of the special features of the '916'report, and also the '797' report, are as follows. First, they are based on analysis of the international literature, and take different types of epidemiological and experimental study into account. Second, they are shaped in order to be the best basis for policies and actions to prevent the range of non-communicable diseases specified.
Third, they are expressed quantitatively, often in the form of ranges of numbers. This is crucial. Only a quantified approach, which in the case of fat, saturated fat, trans fats, sugars and salt relates to amounts considerably lower than seen in most highly industrialised high-income countries, enables rational policies. As indicated above, quantification has been resisted in many official reports issued in the US, and more recently in other countries such as the UK, which show increasing evidence of policies that allow greater commercial freedom, and a more 'industry-friendly' approach to public health. Quantification is also resisted by the food and drink processing and allied industries. They are understandably particularly hostile to the idea that public health will be improved by consumption of foods and drinks other than their products. There is more on this below.
Nutrition: An imperative global issue
Rigorous analyses are now showing that nutrition is ever more important, in determining the state of public health at all levels. Within the last ten years, the relative importance of nutrition compared with all the other factors affecting global health, has been systematically assessed. This reflects a crucial change in analysis and is vital. Nutritionists naturally think dietary issues matter, but then often consider this so self-evident that they retreat to their bunkers, while other health policy experts are able to set out a cogent case and therefore influence politicians and officials. They have identified the scourges of tobacco-induced disease, or malaria, tuberculosis, HIV, infantile pneumonia or diarrhoea, in dramatic, quantified terms. This then comes over as vivid and persuasive, for public policy is political. It is not enough to tell legislators or officials that a problem is important. They will rightly want to know how important it is.
Thus a decade ago, a large WHO body of many different working groups assessed rates of death and disease globally, and calculated the contribution of different risk factors to the development of diseases. Their conclusion was that nutritional factors are the fundamental basis for five of the top ten risk factors underlying the immediate causes of death and disability in the world (4). That was 2002. The latest edition of this work, published in 2009 (5), re-emphasises childhood underweight as the top risk factor primarily in terms of the length of time in years lost through early death, and also emphasises unsafe sex, and poor water quality and sanitation. It has hypertension, suboptimal breastfeeding, high blood glucose, overweight and alcohol, as well as smoking, in the top ten contributors to global disability-adjusted life years. These DALYs are not only life years lost but also years of disability as well. The specific nutritional factors have changed somewhat, following the updating and interpretation of data, but nutritional issues have now shot to the top of the global public health policy agenda. What's needed now is that heads of state and government, and their senior ministers and officials, realise this, and agree policies and actions as clear-cut as those of the Millennium Development Goals. As I will show here, we are a stage short of this at the moment.
The urgency of the need for radical action is amplified by the finding that 80 per cent of the deaths from non-communicable diseases occur in relatively impoverished countries. Infectious and deficiency diseases remain endemic in many of these countries. Nevertheless, these are now already becoming overwhelmed by the escalating burden of chronic diseases whose immediate dominant causes are tobacco, alcohol, and unhealthy diets.
The paths to the road to the summit
The paths that merged to form the road on the way to this month's New York summit have been staked out since 2007. Five can be discerned. I will come to the first one, below. The second is that of governments, as they became aware of the heavy burden of non-communicable diseases, and perhaps most of all the shocking emergence of childhood obesity and early life diabetes, particularly in lower-income countries that remain burdened by infectious and deficiency diseases. The third is that of leading professional organisations concerned with the control and treatment of some but not all major non-communicable diseases, now united within the 'NCD Alliance'. The fourth, more a superhighway than a path, is that of what can be called 'industry' for short, but which really is that sector of the food and drink processing industry, its representative and allied bodies, and associated organisations such as the advertising industry. Food and drink processing is dominated by colossal transnational corporations, many of whose products, consumed as substantial parts of diets, are harmful to personal and public health.
The fifth path is that of relevant United Nations agencies, in particular the World Health Organization, normally the lead UN agency. Experienced, dedicated but grossly understaffed and under-resourced WHO senior officials have struggled to keep hold of the New York summit agenda, which formally is the responsibility of the UN as a whole.
And the first path? I have already referred to this. It is the path of scientific knowledge. To continue the metaphor, it is the path through the fields in which the seeds of research and other investigation are sown, for later travellers to gather the fruits of knowledge, which for us concern the causes of disease, health and well-being. Scientists like to think of this as the straight and narrow path. It has been the path less travelled lately, and the fruits of its fields have been neglected, as I will show later in this commentary.
The 2007 CARICOM initiative
The '916' report ends with a call for concerted international action, co-ordinated by the UN and led by governments. This challenge has been taken up by various member states. These include the Caribbean Community (CARICOM) group of 15 member states, at a special summit meeting held in 2007 in Trinidad at head of government level. The meeting agreed that non-communicable diseases amounted to a public health crisis and that in the Americas the Caribbean was worst affected. Obesity has increased very rapidly. Five member states in the Caribbean region – Barbados, Trinidad and Tobago, Jamaica, Belize and Cuba – have the highest rates of diabetes among all countries in the Americas. Reasons given included globalisation, urbanisation, and 'advertising and propaganda from the North affecting Caribbean life styles' (6).
This led to the Port of Spain Declaration, 'United to Stop the Epidemic of Chronic NCDs' issued in September 2007. (The executive summary for the CARICOM summit is available here as a pdf) This in turn, together with the other initiatives summarised below, led by way of a following meeting of the heads of state of the Commonwealth to the decision in May 2010 of the UN General Assembly to convene a High Level Meeting on the prevention and control of chronic diseases. This is the summit being held this month.
The NCD Alliance: a new force
A broad path to the summit has been laid down by a specially created non-governmental body, the NCD (non-communicable disease) Alliance. This began with an initiative of the International Diabetes Federation (IDF). This is the worldwide representative body of professional associations mainly concerned with the control and treatment of diabetes, and with its prevention usually in the medical sense. In 2006 IDF succeeded in making its World Diabetes Day an official UN occasion.
The IDF then pressed for a conjoint drive with other professional associations to bring the whole issue of comprehensive screening and management of key chronic diseases to the UN General Assembly. It therefore teamed up with the World Heart Federation and the Union for International Cancer Control, and later the International Union Against Tuberculosis and Lung Disease, to create the NCD Alliance. This was launched in Geneva on the occasion of the WHO World Health Assembly in May 2009 (7). The NCD Alliance now states that it represents over 2,000 professional and civil society organisations. It has become an effective campaign supported by Alliance members and associates, with unrestricted grants from the pharmaceutical industry and other sources. The benefits of the Alliance include speaking with one voice on the topic of major non-communicable diseases.
This has however, meant that other organisations with experience in relevant fields, including those with special experience and knowledge of food systems, industry, agriculture, trade, energy, physical resources, justice and equity, environmental impact, and prevention in the full non-medical sense, have been sidelined. Also, from the start, the lead NCD Alliance members have insisted on having only 'their' four diseases identified as the prime causes for concern. Obesity, and other chronic diseases specified in the 1990 '797' and 2003 '916' reports, have been excluded from the Alliance's programme. In its initial statement, just four prevention priority areas were identified as targets for action. These were a tobacco-free world by 2040; reduced harm from alcohol; a rather vague general statement about unhealthy diets and physical inactivity; and just one quantified dietary target, reduction of salt consumption on a population base to 5 grams a day (7).
There has been some friction between the Alliance, and WHO and UN member states who want emphasis to be given to other diseases also, and to primordial prevention policies, involving broad public health measures beyond the scope of the medical and allied professions. The main interests of the Alliance remain those of most of its members. These are disease detection, medical treatment of disease and its risk factors such as high blood pressure, and health care provision. It seeks to revolutionise health service provision, even in impoverished countries. It wants the main focus of the summit and its outcomes to be on more effective medical responses. These include early screening for the four disease areas, and early interventions including drug therapy for biological risk factors such as high blood pressure, high levels of unhealthy blood fats (dyslipidaemia) and high blood glucose levels, so that these conditions can be checked and not lead on to serious clinical disease.
These are of course laudable aims, although it is not clear how impoverished countries and regions will ever be able to afford in the foreseeable future, medical approaches to epidemic diseases at a population level beyond that of the wealthier middle classes. But they are not public health approaches, in the sense of the word that refers to societal change for the better. They do not address the social, economic and environmental drivers of disease and of well-being, and almost by definition cannot have much effect on the prevalence of epidemic diseases. So the NCD Alliance's focus has its limitations.
Transnational industry: 'private partners'
For the last ten years and more, the UN and its agencies, powerful national governments such as that of the US, new massively resourced philanthropies (in particular the Gates Foundation), international finance institutions (notably the World Bank), and powerful champions of big business (in particular the World Economic Forum), have combined in agreeing that the way forward for the improvement of the human lot, including public health, is by means of 'public-private partnerships' with 'the private sector'.
In principle the policy is sensible. Industry certainly must be a partner in the implementation of any public health policy. Partnerships between public bodies including the UN, national, state and municipal governments, and industry as a whole, most especially industries whose interests do not directly conflict with those of public health – the energy, engineering and electronic industries, for example – should be of huge benefit. Thus, redesigning cities so as to make them safe and pleasant for walkers and cyclists, with new and renewed parks and open spaces, and restrictions on private motorised transport, would be a magnificent public health initiative. Indeed, this is being done in a number of big cities, including in lower-income countries. This policy, turned into action, will prevent a substantial percentage of overweight and obesity, diabetes, cardiovascular and musculoskeletal diseases, and obesity-related cancers.
The same also should be true of partnerships between public bodies, and the food and drink industry as a whole. This includes producers such as farmers and growers, manufacturers, distributors, retailers and caterers. One potential benefit of such partnerships would be policies and actions that would, over time, transform food systems so as to maximise production and thus consumption of fresh, minimally processed and other healthy foods and drinks. Another benefit would be policies and actions to protect and preserve healthy traditional and established food systems and other relevant public goods. A rational approach to such partnerships would include caution in the case of those industry sectors whose commercial interests are in direct conflict with those of public health. This could be resolved in ways similar to those that have been used by WHO in its dealings with the alcohol industries (8) (pdf available here), or by giving them observer status and including them in policy implementation but not in its formulation.
However, the 'private sector' 'partners' that have engaged with the process leading up to this month's summit have overwhelmingly been and are the gigantic transnational food processors and allied trades whose products are unhealthy, and even toxic in the classic sense, with increasing evidence of addictive properties, together with their representative and supporting organisations. To the best of my knowledge and that of others in a position to know, neither the UN as a whole, nor WHO or other UN agencies, has made any serious attempt to engage non-conflicted industry, outside or inside the food and drink sector, in the process leading up to the summit. Quite the reverse. Despite constant protests and warnings from independent organisations and witnesses, the UN collectively seems to have assumed that the only suitable 'partners' from the 'private sector' are industries whose interests are generally hostile to public health. Indeed, it almost seems that in use, 'the private sector' is a code-phrase for 'transnational food and drink processors and their associated and supporting organisations', in which case it would be more transparent to say so.
Thus, those industries whose products are a direct cause of the global public health problem are being invited – or have invited themselves – to be part of its solution. Jaundiced commentators have compared this with bomb manufacturers being invited – or inviting themselves – to engage in and to direct the business of arms limitation talks. Such vivid analogies aside, I have yet to meet anybody outside this process who, being informed of it, at first is able to believe what I am saying. But it is true. As now interpreted and operated, the so-called 'public-private partnerships' are against the public interest and that of public health.
There is more. Even worse, executives from the World Economic Forum, from transnational food manufacturers and their umbrella bodies, and industry-driven bodies such as the International Business Leaders Forum, have been playing a leading part in setting agendas and managing the business of some of the official meetings leading up to the New York summit. Perhaps worse yet, in this period, including this year, some senior UN officials with vast networks and knowledge of public policy and practice have been taking senior executive positions in transnational food and drink processing corporations. This they claim is justified because - they say - they can then help to enlighten these industries.
The food and drink business is now the biggest industry in the world. The turnover of the biggest individual transnational food and drink companies is much the same as the gross national product of entire nation states in the mid-range of scale such as Sri Lanka, Slovenia and Tunisia. It is also extremely powerful. Chief executive officers of the biggest industries command discretionary funds amounting to $US billions available to them to use at any time. The scale of the food industry is inevitable given that everybody on earth needs to consume adequate amounts of food. Industry executives know that when products taste good and are habit-forming, their profitability depends on manipulating their cost and price, making them available wherever possible, and marketing them intensely. By these means they increase their sales and thereby change population behaviour. The policy of the transnational food and drink processors is above all to ensure that their companies and their branded products are major players, especially in lower income countries whose populations are large and growing, and most of all those with a rapidly increasing urban middle class with disposable incomes. In this way transnational industries can rapidly increase their volume of sales: their future profitability depends on penetrating these lower-income markets aggressively.
No wonder that major non-communicable diseases are now pandemic. The world's entire population, perhaps apart from rural farmers, destitute urban and rural communities, and other groups with little money, is now being trained in habits of constant consumption of unhealthy products, many of which are in ready-to-consume snack form, of which many are marketed ruthlessly to children. These are all rapidly increasing the profits of the food producers and the corporate affairs, public relations and advertising industries.
These are reasons why the transnational food and drink processors are so heavily and successfully engaged with the UN non-communicable disease process. It is also no wonder that documents prepared in preparation for this month's summit contain practically no statements or recommendations that could have a significant adverse impact on the short-term sales or profits of transnational food and drink processors.
It is important to emphasise that these giant corporations are only one part of the food industry as a whole. The livelihoods of other sectors of industry, including co-operative family farmers and other primary producers, and national and smaller manufacturers, are jeopardised by the activities of transnational corporations. The activities of the transnationals undermine, damage and even may destroy national and local food systems, businesses, economies, employment and livelihoods. They make impoverished populations vulnerable to financial speculator-driven spikes and erratic fluctuations in the prices of food commodities and of food in the shops. Their intense monotonic approach to exploiting resources depletes soil and water and energy resources. None of this is a matter of serious dispute. They also contribute to the global environmental 'footprint' that is now heavier than can be sustained by global resources (9).
It also needs to be emphasised that the immediate commercial imperatives of highly capitalised industries, driven as they are by market ratings, share prices, speculative investment, and the ambitions of their current chief and senior executives, are not necessarily in the longer-term interests even of those industry sectors, let alone industry as a whole. As a previous director for 17 years of the largest agriculture and food research institute relating to nutrition in Europe, and as such with a responsibility for the long-term welfare of a flourishing national food producing industry, I think I can make this point with some authority.
The UN: established and new thinking
The public health needs and priorities of the world's regions and nations, as represented by their governments, vary. These are different in nature from the needs and policies of international and national professional organisations mainly concerned with the treatment of disease. Both are different from those of the transnational food processing industries and their associates. All are different from the purposes of the United Nations and of the various UN agencies concerned in one way or another with public health and the prevention and control of diseases and disabilities. Because of the positioning of the summit as a UN General Assembly event, both the UN secretary general's office and the WHO director general's office have been engaged with preparatory documentation, together with officials from Jamaica and Luxembourg, the two member states with lead responsibility. Given all this, it is remarkable that a superficially coherent draft Political Declaration has been produced by the UN secretariats.
WHO has formally remained the lead UN agency responsible for preparations for the summit. Pressures on its officials have been extraordinary. They have had to take into account new urgent demands, not all consistent, and perhaps above all the overall requirement, specified at UN secretary general level, that 'the private sector' be fully engaged as a partner in the process.
That is not all. In recent years, a series of commentaries have been published by influential journals, notably The Lancet, often co-authored by experts who have worked within the UN system, offering new analyses. One common theme has been that programmes designed to prevent and treat disease should be cost-efficient and preferably pay for themselves, or even be seen as economically beneficial in the sense of 'making a surplus' in terms of gains in productivity. In making such calculations, some of which involve 'heroic' assumptions and extrapolations, much depends on what is counted as cost and what as benefit. Such 'best buys' have been given a new priority. As a result of all this, much of the foundation work for policies and programmes designed to prevent non-communicable diseases, built up over the last 30 years and more, has been ignored, neglected, or dumped. New generations of policy analysts and makers have emerged, whose insights, often brilliant, have sometimes overlooked or ignored long established solid evidence in favour of novel notions with only a modest or even fragile evidential basis. Again, more of this later in this commentary.
The Lancet paper
This year WHO published a new survey of global health status (10) (available here as a pdf). This is designed to set out the scale of the issues confronting all the actors involved in this month's summit. In April The Lancet published a very important and highly influential paper (11) (available here as a pdf) co-authored by 44 scientists, officials and policy analysts, positioned as The Lancet NCD action group together with the NCD Alliance. The paper's first two authors, Robert Beaglehole and Ruth Bonita, recently held senior positions at WHO. The paper sets out policy priorities for NCD prevention. Its overarching priority is a world almost free from tobacco by 2040. It proposes a target of an annual NCD reduction of 2 per cent. It strongly recommends alcohol control using measures affecting price, promotion and availability. Its main dietary recommendation is salt reduction. It also recommends policies designed to reduce saturated fat, trans fat and sugar in processed foods, emphasising the need to reduce consumption of sugared drinks. In a key passage, the paper says: 'Strong government encouragement, including regulatory and fiscal measures, will be needed'.
The Moscow Declaration
Later in April, a conference at ministerial level was held in Moscow, preparatory to this month's summit. I was invited to be one of the participants at this meeting. A Moscow Declaration was issued (12) (available here as a pdf). This drew on the WHO global health status survey (10). It states that 'a paradigm shift is imperative in dealing with NCD challenges, as NCDs are caused not only by biomedical factors, but also caused or strongly influenced by behavioural, environmental, social and economic factors'. It includes a call to 'control tobacco, the harmful use of alcohol, and reduce salt', and also mentions 'promotion of healthy diet, physical activity and reduction of obesity (decreased consumption of fat, trans fats and sugar)'. It endorses collaborations involving 'the private sector'. It also specifies 'implementing cost-effective policies, such as fiscal policies, regulations and other measures to reduce... tobacco use, unhealthy diet, physical inactivity and the harmful use of alcohol'.
The Moscow Declaration includes no explicit reference to quantified time-based goals. It does however, reference various policies already endorsed by member states at WHO meetings, and thus formally already in place. One is the 2004 Global Strategy on Diet, Physical Activity and Health (13), a statement of general principles. Another is the 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases (14). This does mention legislation and fiscal measures. Its title indicates its time-frame. It specifies the need for 'reducing salt levels, eliminating industrially-produced trans fatty acids, decreasing saturated fats, limiting free sugars', without indicating amounts other than in effect for trans fats. Industry is usually comfortable with recommendations that exclude numbers, because these can be taken to mean almost anything. The third document commended is the 2011 Global Strategy to Reduce the Harmful Use of Alcohol (15), which states clearly the need for statutory and fiscal measures.
The WHO 'targets' paper
In July, close to the New York summit, WHO released a short 'targets' paper (16) (available here as a pdf) It was designed as a consultation document to be discussed with UN member states by email forum. This is more purposive. It proposes that by 2025 there be a 25 per cent relative reduction in the four diseases represented by the NCD Alliance, as indicated by deaths between the ages of 30 and 70. Its main focus is on disease end-points and screening although some risk factors, for example hypertension and obesity, are included. It recommends an overall reduction of 10 per cent in alcohol consumption and reduction of population salt consumption to below 5 grams a day. On general diet it recommends elimination of partially hydrogenated vegetable oils from food systems, and thus elimination of industrially generated trans fats. It finally specifies 'no marketing of foods high in saturated fats, trans fatty acids, sugar or salt to children'.
The NCD summit draft Political Declaration
I now turn to the Political Declaration due to be finally discussed and agreed at the New York summit this month. Successive drafts have been circulated or disclosed. (Again, here is a recent version in pdf form) Most of my remarks that now follow use this draft Declaration as a basis. At the time of writing, it seemed likely that any changes to the draft would be in the direction of keeping it general and if anything making it less pointed. It contains few references to statutory policies and then only as a possible option for member states. It contains no quantified targets, either for time-scale, or for reduction in disease, or for changes in dietary patterns. Partly for this reason, it is being furiously denounced by the NCD Alliance. There are other reasons to see the Declaration as problematic. These follow below.
Tobacco: Still under control
The WHO Tobacco Framework Convention, agreed by UN member states as legally binding, is a highly effective tool for reducing smoking, use of tobacco, and exposure to tobacco smoke. It is based on recognising the fundamental importance of restricting availability of products to all children, limiting outlets to adults, prohibiting smoking in many public places and offices, taxing the products heavily, forbidding all forms of marketing, and compelling industry to include increasingly prominent and explicit warnings on packages and advertising. It is vital in itself and also as a guide to other policies and actions that will effectively protect public health.
In the draft Political Declaration, there is no suggestion that policies and approaches to smoking and other uses of tobacco be changed. The Tobacco Framework Convention remains unchallenged and intact. Concern that its measures may amount to a regressive tax that would be of special disadvantage to impoverished people, an argument that has been favoured by the cigarette industry, is not mentioned. There is no sign that the New York summit will modify UN policies here, or recommend that member states modify their policies. This is as should be expected, but should be mentioned, and is all to the good.
Alcohol: An opportunity ducked
What is current policy of the UN to alcoholic drinks, and to the alcohol industry and its associated organisations? Examination of the documents prepared for the New York summit, including the draft Declaration, does not yield a clear answer.
Alcohol is not a product that is necessarily always harmful in any quantity, as is tobacco. But it is toxic. It is identified by the International Agency for Research on Cancer, a specialist agency of WHO, as carcinogenic. It is correctly identified by WHO as an 'intoxicating and dependence-producing psychoactive substance' (8). Perhaps for this reason it is often omitted from reports and policies concerned with food, nutrition and health. But for those who drink, alcohol is a part of their diet. In addition to its place as part of meals and social occasions, alcohol is widely consumed in order to influence mood, behaviour, and social interaction.
A study published in The Lancet in 2009 (17) estimated that worldwide alcohol causes 3.8 per cent of all deaths, amounting to nearly 2 million a year. Alcohol-related causes of death include homicide, suicide, violence, arson, poisoning, accidents, stroke, and oral, breast, colorectal and liver cancers. It is estimated to cause the loss of 4.6 per cent of all disability-adjusted life years (DALYs). The study judged that alcohol is as great a menace as tobacco smoking was a decade previously. It also noted that women, particularly young women, are now drinking a lot more alcohol.
Excessive consumption of alcohol has immediate and easily observed effects which are so undesirable, that political measures along lines similar to those used to control tobacco use designed to restrict its use, and also to encourage moderation, have wide popular support. Proposals concerned to protect public health should emphasise the need to reinforce statutory and other formal measures designed to limit availability, affordability and consumption of alcohol, and include quantified goals. They should also state that in those parts of the world where consumption of alcohol is forbidden, laws to this effect should be upheld.
As has happened in the past with tobacco, what has emerged with alcohol, as a prelude to policy making for the New York summit, is a battle between utterly convincing scientific and medical evidence, backed by public opinion, and in many countries supported by strong statutory regulation on the one hand, and on the other hand, intense lobbying by the alcoholic drinks industry. The alcohol industry seeks to minimise restrictions on marketing, control of alcohol outlets and additional taxes. Its aim is that statutory restrictions on price be eased and on availability be abandoned, in favour of ineffective information and education programmes, industry self-regulation, no warnings on labels, inconspicuous information on alcoholic content, alcoholic drinks available in shops that stay open 24 hours a day and 7 days a week and in late-night bars, cheap and discounted alcoholic drinks and 'alcopops' and other 'starter' drinks on prominent display, leaving governments to use public money to crack down on binge drinking and alcohol-driven mayhem. In many countries many and most of these policies are in place.
Happy hour at the UN?
So what is the attitude of WHO? Within the last five years its view of alcohol seems to have become more focused in terms of its hazards, and yet at the same time somewhat more permissive. In 2006 the policy of WHO included a rule that 'interaction with the alcohol industry should not lead to or imply 'partnership' [or] 'collaboration' (8). This policy now seems to have been modified. The alcohol industry, or at least its associated organisations, now seems to be part of the general UN policy to foster 'public-private partnerships'. I am not aware of any recent statement to the contrary, and organisations linked with the alcohol trade have been involved in some of the preparations for the New York summit.
As with the tobacco industry, public health professionals have discovered that when industry objects vehemently to some proposed regulatory measure, this is a pretty sure sign that it is likely to be an effective way to restrict sales. So, what actions are appropriate? The WHO 'targets' paper (16) recommends, of alcohol, by 2025: '10% relative reduction in per capita consumption of alcohol; and 10 per cent relative reduction in prevalence of heavy episodic drinking'. But this modest goal omits to pay any attention to factors that drive overconsumption and abuse of alcoholic drinks. Governments throughout the world already act on the conclusive evidence that statutory regulations that increase the price of alcoholic drinks, and that restrict their marketing and availability, reduce consumption.
Unfortunately the draft Political Declaration evidently ignores the WHO 'targets' paper, despite this being designed for consultation with member states. In a standard vague phrase, it occasionally mentions 'the harmful use of alcohol'. It includes no goals for reduction of alcohol consumption, but it does include a reference to the 2011 WHO Global Strategy to Reduce the Harmful Use of Alcohol (18). This Strategy, itself agreed only after intense debates, emphasises the value of education and information, despite acknowledging that by themselves these approaches are not effective. However, it does recommend formal measures, and states that policies need to reach beyond policy-makers concerned with health and also engage those concerned with 'development, transport, justice, social welfare, fiscal policy, trade, agriculture, consumer policy, education and employment'. Indeed so.
The need for specific policy and action
The draft Declaration does not reference the WHO Global Status Report on Alcohol and Health, launched this year in February (18). It should. This sets out ten ways to reduce the damage done by alcohol, and is specific about what should be done. 'Measures controlling the availability of alcohol include age limits for the purchase and consumption of alcohol, monopoly or licensing systems for alcohol distribution, bans on the sale of alcohol at petrol stations, and limits on the hours and days that it can be sold. Pricing policies focus on alcohol tax revenues as a percentage of total government revenues, and the existence of dedicated alcohol taxes. Drink-driving policies include blood alcohol concentration... laws and random breath testing. Policies on alcohol marketing include ... bans on product placements and sports sponsorships, and limits on retail sales below cost. The existence of warning labels on alcohol advertising and containers is another policy'.
These measures, now standard practice in many countries, need to be strengthened. None of this is set out in the draft Political Declaration. Apart from the reference to the WHO Global Strategy (14), the closest it comes is in a passage suggested by the 'G77' group of lower-income member states, which recommends to 'increase policy measures to regulate... availability, price and marketing of alcohol', supported by New Zealand and Norway. Another suggested addition refers to 'globalization of trade and marketing' including of alcohol. Whether these suggestions survive to the finally agreed document, remains to be seen.
This is not a time to go easy on alcohol consumption and on the alcohol industry. So far the opportunity to make firmer statements has apparently been ducked.
Omission of children
Concerning alcohol, the worst feature of the draft Political Declaration – and indeed the 'targets' paper (16) – is that proposed policies for the advertising and marketing of food and drink products to children, refer only to non-alcoholic drinks. There is no reference to the marketing of alcohol to children and young people. See Box 1. It is reasonable to conclude that this is a result of intense and so far successful lobbying by the alcohol industries and their representative organisations.
Box 1
Alcohol and adolescents
The importance of alcohol misuse in young people is being overlooked, despite the fact that alcohol has shot up the list of global public health problems.
A total of 27 per cent of the world's population is aged 10-24 years. In the new WHO 2011 analysis of the global burden of disease for alcohol and health (18) the total number of incident DALYs (disability-adjusted life years) in this age group is about 236 million, representing 15·5 per cent of DALYs for all age groups. Africa has the highest rate of DALYs for this age group, 2·5 times greater than in high-income countries (208 in contrast with 82 DALYs per 1000 population). Across regions, DALY rates were 12 per cent higher in girls than in boys between 15-19 years (153 in contrast with 137). The main single incident DALYs in 10-24 year-olds are alcohol (7 per cent), and then four factors three of which are related to alcohol consumption: unsafe sex (4 per cent), iron deficiency (3 per cent), lack of contraception (2 per cent), and illicit drug use (2 per cent).
Any rational global public health policy needs to get serious about the damage being done to children and young people by alcohol, and impose stringent statutory restrictions on its availability and affordability. All restrictions and prohibitions concerning the advertising and marketing of food and drink to children and young people must also include alcoholic drinks.
Obesity: The elephant in the room
Now follow a series of sections on foods, nutrients, and (non-alcoholic) drinks. These are different from tobacco and alcohol. We can all live lifelong in good health without tobacco or alcohol, but food is a necessity. For this reason many commentators immediately highlight the different approaches needed. One cannot 'ban eating' and of course nobody has ever suggested such a thing!
But many policy-makers these days go to an opposite extreme, and in effect say that because food and drink are essential, it would be wrong and even absurd to support international and national regulations designed to modify or restrict consumption in any way. Instead, they say, individuals can be encouraged to make suitable food 'choices'. This 'information and education of consumers' approach is very evident in the draft summit Declaration. As shown in analyses such as that recently published by the OECD, use of the media to inform and educate people is almost useless. It is nonetheless much favoured in countries whose governments favour the removal of regulations designed to protect public health and public goods, which may impede big business. What this fails to recognise, is that while on the one hand food is essential for life, and much food and drink is healthy or harmless to health, many aspects of industrialised diets are harmful to health, and some of these are in a real sense addictive or toxic, or both.
Obesity is a non-communicable disease
The most blatantly obvious ill-effect of unhealthy diets, at first in high-income countries, and now in most countries, is overweight and obesity, which is now an uncontrolled pandemic, including among children and young people.
When I began to draft this commentary, I thought that I would not mention that obesity is omitted from the list of non-communicable diseases specified for the New York summit. Since obesity is non-communicable, is classified as a disease, and as well as being a serious and even directly life-threatening condition also increases the risk of diabetes, heart disease, common cancers and other diseases, the omission is obviously ludicrous, and of itself has already brought the summit into some disrepute.
But I have an interest, as founder and first chair of the International Obesity Task Force, the partner with WHO in its first '894' report on the prevention and management of obesity (19), and now as president of the International Association for the Study of Obesity. Having declared my interest, here follow a few remarks.
Omission of obesity presumably is because it is not of immediate professional interest to the organisations that form the NCD Alliance. There are now very few effective drugs for treating obesity. This is not a good reason. The science showing that energy-dense processed products and sugary soft drinks, consumed in typical quantities, are an important cause of obesity, is increasingly being validated by independent studies. The manufacturers of 'fast' and ' 'convenience' snacks and drinks that are 'partners' in the summit process must feel more comfortable, not being faced with the laughable task of explaining that obesity is all about physical inactivity and is averted by making sensible choices within 'a balanced diet' and has nothing to do with their products. It is easier for them not to be confronted with questions concerning obesity.
Examination of the draft summit Declaration shows that the UN secretariat and UN member states, perhaps spurred by many speakers at meetings convened by member states, have now made considerable attempts to bracket obesity with the 'official' non-communicable diseases, and to mention other diseases also. Good. Let us hope that the proposed revisions and additions to early drafts so far proposed survive. The extra addition needed, is to include obesity as a fifth non-communicable disease. Others such as those covered in the '797' and '916' reports (2,3) could also be included.
A spur to these revisions has now appeared in the form of what amounts to a special issue on obesity of The Lancet, published on 27 August as I write. This includes an editorial (20) and a series of papers, two of which, coauthored by Boyd Swinburn, one of my successors as IOTF chair, are referenced here (21, 22).The editorial states: 'Sadly, the forthcoming high-level UN meeting on non-communicable diseases is marred by the reluctance... to set targets. One immensely important next step in the fight against non-communicable diseases could be the agreement on a [legally binding] framework convention on obesity control. Who will take the lead?'
Energy-dense food products: Missing
So, what about high energy density, a quality of very many processed products produced by transnational food manufacturers that is a cause of overweight and obesity, beyond any serious dispute? The term 'energy density' does not appear in the draft Declaration. Nor does any similar term. Furthermore, the draft makes no explicit reference to food processing, except in discussion on trans fats. The implication is that with this exception, any type of food processing is fine. 'Foods with a high content of fat [or] sugar' are mentioned several times, as a suitable case for 'measures' on advertising to children. This makes no distinction between very nourishing foods that are high in fat (such as olives and nuts, for example) or that are sweet (such as many fruits) on the one hand, and on the other hand highly processed snacks and other fatty or sugary products made with degraded ingredients and formulated so as to be habit-forming.
The concept that energy-dense processed food products are a key cause of overweight and obesity and related serious diseases is robust in terms of careful physiological studies on energy balance and the routine increase in spontaneous or 'passive overconsumption' of energy when more energy-dense foods are consumed, as a classic paper by Andrew Prentice and Susan Jebb shows (23). James Stubbs's work shows that foods that include a lot of refined carbohydrates simulate the impact of fat on energy density and its effects in increasing energy intake (24). There is not yet a comprehensive set of epidemiological studies on this topic, perhaps because the concept is so obvious that funders and investigators lack interest!
Sugared soft drinks: Nothing
The draft Declaration never mentions caloric soft drinks, sweetened with sugar or syrup. It could perhaps be said that sweetened soft drinks are indicated in that part of the draft Declaration that mentions the policy option of limiting the advertising and marketing of foods 'with a high content of sugar' to children. But this would be a thin rationale, impossible to defend. The huge and increasing volumes of high-calorie soft drinks consumed by people of all ages are of immense concern. The evidence that soft drinks, and in particular cola drinks (known as 'soda' in the US) are an important cause of overweight and obesity, is now generally agreed by independent expert groups to be incontrovertible. In addition to their caloric content, they seem to by-pass normal mechanisms of energy homeostasis. These days the soft drink industry and its trade associations have almost abandoned their attacks on the independent science that proves this point. The issue should have been headlined in the Declaration.
Baby formula: Not a word
Perhaps the most important development in understanding of the causes of non-communicable diseases that has taken place in this century, is that the pathology of these diseases begins early in life – and even before birth. It follows that the important contributors to the prevention of these diseases impact during pregnancy, infancy and early childhood. After weaning, the best diet for children is much the same as that for older children and adults. In the first six months and preferably longer, the best protection is given by breastfeeding. This is mentioned a couple of times in the draft Declaration. At one point Norway, with support from Mexico, Australia and the EU, proposes the phrasing 'Promote, protect and support breast feeding, as breast feeding' [which is to say, being breastfed] 'is essential in the prevention of obesity as well as under nutrition'. The draft Declaration omits to mention that lactation protects against breast cancer in the mother, as well as being breastfed protecting against overweight and obesity and related diseases in the child (25).
But the draft Declaration never mentions baby formula. This, with energy-dense weaning and post-weaning diets, is a cause of overweight and obesity and therefore related diseases. Baby formula also massively increases the risk of diarrhoeal diseases and other serious infections, and deficiency states, most of all in lower-income countries, and in particular where water supplies are unsafe. Why its omission? Given that the biggest food and drink manufacturer in the world is also the leading manufacturer of baby formula, perhaps the summit Secretariat felt it would insensitive to do so. Whatever the reason for the omission, this is not in the interests of public health.
Salt: Named, but no number
Reduction of salt, especially as contained in processed foods, is given high priority in reports and papers prepared with the New York summit in mind, as a 'best buy' that should show a very substantial economic surplus (11). Salt reduction is no longer seriously disputed by food manufacturers and caterers. There have been some attempts to question the evidence that salt promotes hypertension and cardiovascular disease, but these objections are usually made by the salt industry, or by scientists who are close to the industry or to manufacturers whose profits depend on extensive use of salt.
What manufacturers do not want, is a number. They want to remain free to reformulate their products in their own time, and to reduce salt by amounts they consider to be commercially safe. Many salty snack products are being aggressively and successfully promoted in lower-income countries, and in some cases are achieving 'double digit growth', meaning additional annual sales of over 10 per cent. It therefore is perfectly possible that successfully marketed lower-salt snacks will overall increase salt intake, as snack consumption rises.
Outside of any industry-influenced arena, the figure on a population basis of a maximum of 5 grams of salt a day has been agreed for many years (2,3). This is policy in many countries, as shown in a new review in the British Medical Journal (26). Will this or any number for salt appear in the summit Political Declaration? As I write this is disputed. A previous draft had the number of 5 grams suggested by Norway, the inveterate champion of good causes. The draft examined here has no number, which at least has the merit of being consistent with no numbers for anything else! It may be that the secretariat does not wish to have the obvious anomaly of a number for salt, but none of the numbers for other constituents of diet that have been endorsed again and again for decades! On 21 September we will see if there is a number for salt, or for any dietary constituent. An educated guess is that there will be no numbers for anything, in a document framed as a statement of general principles.
What we eat: Do we choose?
I now come to two sections of this commentary in which I include recent highly significant evidence on behaviour. Both sections refer to studies whose findings are not convenient to industry. These do not figure in the draft Declaration or, as far as I know, in any other documents prepared for the New York summit.
Policies to prevent disease and improve health that largely rely on information and education of the customer and consumer have given priority by the governments of many if not most countries for several decades. The draft Declaration evidently assumes that these are the appropriate policies. They derive from the notion that people should be free to make their own individual choices. Industry favours this approach, which is particularly helpful to those companies manufacturing products that are marketed on the basis of manipulating population choices and inducing practically unconscious habits. The doctrine of the supremacy of individual choice is an ideological position. The idea that left to themselves, or perhaps guided by labels and pamphlets, people will make healthy choices, is obviously contradicted by the rapid rise in obesity, diabetes and other diseases related to consumption of unhealthy products, and in any case has little if any good evidence to support it.
There is now good evidence that eating behaviour is mostly automatic (27). Much of what people purchase and consume is actually not a result of real choice. This is obviously the case with products which people are progressively trained to consume habitually. But a recent review co-authored by Deborah Cohen goes further. It states: 'the amount of food eaten is strongly influenced by factors such as portion size, food visibility and salience, and the ease of obtaining food. Moreover, people are often unaware of the amount of food they have eaten or of the environmental influences on their eating'. The review goes on to say: 'A revised view of eating as an automatic behavior, as opposed to one that humans can self-regulate, has profound implications for our response to the obesity epidemic'.
Indeed it does. This may be news to us, but it is very well-known to industry. For example, the big food manufacturing and retailing industries use many sophisticated techniques that determine design of the packaging and the positioning of foods at different levels, based on monitoring subconscious attractiveness of different labels. Industry research involves volunteers wearing devices that automatically track eye movements and thus pick up the subconscious microsecond long monitoring of different labels. It is also now almost routine for big players in industry, in checking on food taste and flavour, to track with brain scanners the responsiveness of the brain pleasure centre.
This approach has been and is used by leading liquor and other alcoholic drink manufacturers, in order to convert what was once the very low alcohol consumption of young women to what are now dramatically increased levels. The technique involves using tasteless vodka with cocktails of chemical flavourings added, designed to pick up favourable brain pleasure responses in young women at different stages of their menstrual cycle. Amplified by marketing, alcohol drinking in young women has escalated, and is now a major public health problem (15,17,18).This crisis is clearly at least in part caused by the innovative industrial technologies that are circumventing normal behaviour and creating behavioural changes through subconscious methods.
Similar techniques have been and are being used to change behaviour at a whole-society level. Thus, snacking is now taken to be normal. It is no longer strange to see people walking the streets carrying containers of coffee and snacks, even consuming the products as they are walking. A new development is for young women to carry bottles of 'designer water' wherever they are, as a sign of sophistication.
Brain growth: Still immature until 18+
In considering restriction of advertising and marketing of food products to children, up to what age should young people be considered as children? Analyses relating to acceptance of marketing messages, for example by the US Institute of Medicine (28), specify that evidence is very consistent for children up to the age of 12 years. So this has been the age chosen by many industrial and government groups. Some industries whose products are designed to appeal to younger children specify a top age of 6 years.
However, there has always been evidence showing that older children are susceptible and even vulnerable to marketing influences, and other groups consider that the cut-off should be at an older age, with some invoking the age of 18 years as this would conform with the UN definition in its declarations on the rights of the child. Any suggestion to raise the age at which young people are defined as children has of course been vehemently opposed by industry. This suggests that big firms are well aware of the impact of their marketing to adolescents. There is sound evidence relating to the ability of adolescents to make appropriate judgements on their food choices. Some of this is summarised in Box 2.
Adolescent brain development
The brain of the child and adolescent goes through a range of major biological adjustments. These include a transformation in cognitive understanding, from a straight processing of facts before the age of 12 years, to a slow progression to abstract thinking starting between 12 and 14 years.
Imaging studies show how the brain develops during childhood and adolescence. The frontal part of the brain continues expanding and forming up to the age of about 18 years, when the process of abstract reasoning and appropriate decision making can dominate. Thus the ability to voluntarily inhibit responses to irrelevant stimuli, a fundamental component of cognitive control, has a protracted development through adolescence
It is well recognised by policy-makers in government, the academic community and also no question also by industry, that adolescents' behaviour in relation to alcohol, smoking and drugs reflects these immaturities. Moreover, the result of these behaviours can themselves have very damaging effects on the brain. Furthermore, behaviour that develops during adolescence endures. This means that the conditioning by the environment or cultural setting of adolescents is exceptionally important. Thus the younger people are when they take up smoking, the longer smoking persists. Adolescents have intrinsically little capacity to resist and are very impressionable. Socio-economic factors and change therefore particularly affect adolescents. Any commercial company that wants to maximise its sales of food and drink products will therefore give extraordinary priority both to children and to adolescents.
About half of the world's population now is below the age of 25 years. About half of the world's adolescents now live in Asia with the largest group living in India. Overall 10 per cent of adolescents worldwide smoke or chew tobacco. This figure rises to about 20 per cent in the Americas and the Pacific region. Currently, at least 10 per cent of the adolescents worldwide are overweight or obese. This figure is projected to rise rapidly.
Box 2
The age at which the human brain matures
Any proposal that advertising and marketing of food and drink products to children needs to be restricted, needs to specify the age up to which young people are defined as children. The voluntary guidelines devised by industry usually specify up to 12 years of age, or sometimes 6 years. But new findings strongly suggest that the appropriate age should be around 18 – the age now usually identified as that of general maturity.
Developmental improvements in inhibitory control seem to be supported by age-related increases in effective control by the frontal region of the brain operating on the oculomotor and subcortical regions (29). Mental tests of adolescents, correlated with the connectivity of multiple frontal regions of the brain, show how proper reasoning and mature decision making depends fundamentally on the physical myelination of new pathways to produce functioning connectivity between those parts of the brain that are mature only in very late adolescence. Thus maturing of the neural circuitry with growth of the prefrontal cortex, limbic system structures and white matter association fibres during this period, have therefore been linked with more sophisticated cognitive functions and emotional processing.
These control functions support mature goal-directed behaviours. They show a progressive refinement through adolescence into adulthood, relating to the well characterised distributed neural network. The immaturities of adolescence are therefore now helping to explain the risk-taking behaviours, mood swings, emotional responses and irrational, impulsive thinking, which are part of the normal manifestation of a maturing brain.
Studies of the maturing brain of adolescent girls and boys also show marked differences, with girls maturing somewhat earlier but with different regional brain developments. Differences in activation patterns, with girls showing bilateral and boys only right prefrontal response, may underlie gender-related influences on behavioural responses to affect and emotion. Adolescents as a group are described as showing increased 'activity from the bottom-up emotion processing centers….suggesting that they are more likely to be influenced by emotional context than adults. As a result, poor decisions are often made in states of emotional reactivity'(30). The evidence also suggests that adolescents have a limited ability to assess the outcome of potential rewards, and react much more when anticipating reward compared with adults.
Figure 1
Brain maturation between ages 7-30
Study of 238 subjects using functional magnetic resonance imaging (31)
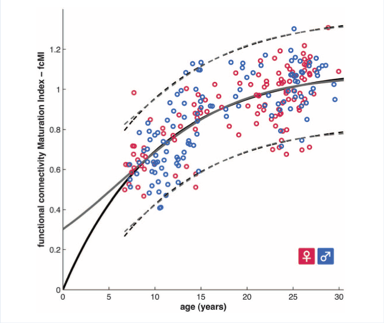
These remarkable new studies on brain reactivity and behaviour in adolescents, done by a large team and published in Science (31), highlight their vulnerability to external influences and their difficulty in navigating an increasingly complex psychosocial environment. The developmental imbalance is unique to adolescents, as children have equally immature limbic and prefrontal regions, while adults benefit from fully developed systems. This explains why adolescents make risky decisions. Their early maturing limbic systems drive choices that seek immediate gratification rather than long-term gains. Some adolescents are much more emotionally vulnerable than others and this again seems to relate to their different rates of brain maturation.
Functional magnetic resonance imaging techniques are now able to assess the maturity of the brain by assessing indices of connectivity. Figure 1 shows that on the basis of these tests the brain is not fully mature until about the age of 25 years .
A rational policy on advertising and marketing
The evidence here, including that summarised in Box 2, shows that the current policy to limit marketing of any product to children below the age of 12 years is clearly inadequate. The upper age limit should be at least 18 years. There is a need to ban all forms of marketing to these vulnerable young people who now represent a huge proportion of the world's population.
Moreover, all forms of marketing, to all age groups, need to be examined with public health as the over-riding priority. New subtle but pervasive forms of subconscious marketing are manipulating the food choices of most if not all exposed adults. This implies the need to consider seriously the approach used in France, where all forms of marketing of high fat, sugar and salt products are subject to regulation, with the use of taxes and health warnings.
Currently the advertising and marketing industries are rogue traders, out of control. There is now need to affirm the same approaches to nutritionally unsuitable foods and commodities as to tobacco and alcohol.
Fats: In the firing line
I now come to the three final sections of this commentary, and then to its conclusion. The sections that follow are about three aspects of dietary fat. These are trans fatty acids (or trans fats), saturated fatty acids (or saturated fats), and total fat. As I complete the commentary, these all evidently remain 'battlegrounds' in the draft Declaration. Because of their importance, I have included more detail than in previous sections. I have flagged my concern earlier in the commentary. This is that the text in documents preparatory to the Declaration, and in its drafts, designed as a basis for public health policies and actions at global level, seems to derive from views on the relative importance of different types of dietary fat that have only a modest or even fragile evidential base, and that conclusions that are solidly based on decades of scientific investigation have been sidelined.
It's hard to guess to what extent this will be the case in the final Declaration, because its draft includes a number of competing proposals and suggestions. The whole draft has 57 clauses. References to 'unhealthy diets' or 'unhealthy foods' are frequent, but any indication of what these terms might mean, starts with the intensely contested clause 38 on page 15-16 of the 28 page draft. One option offered is 'foods high in fat, sugars and salt'. Another suggests 'replacing saturated fats and trans-fats in foods with monounsaturated and polyunsaturated fats', but the EU has placed brackets round 'saturated fats' as well as 'monounsaturated fats', which seems to indicate that this bloc of member states wants these terms removed. A note of 'important issues' in clause 38 includes 'US: listing all the different types of salt fat etc text will be too long', with apparent agreement from Australia. New Zealand suggests for clause 40, 'substantial reductions in levels of trans fats and saturated fats, salt and refined sugars'. Passages on labelling in clause 42 mention fats and trans fat. One option for clause 40 on advertising and marketing to children at one point refers to foods 'high in saturated fats, trans-fatty acids, free sugars or salt' and at another point to foods 'with a high content of fat, sugar or salt'. Other passages are crossed out, presumably meaning that they are cancelled.
What to make of this? First, it is revealing as well as highly depressing that the entire draft makes no attempt to state or indicate what constitutes healthy diets. There is nothing about healthy diets, meals or food. The language is all negative. Second, as already mentioned, there is practically no attempt to distinguish between fresh and minimally processed very nourishing food, and heavily processed degraded products.
Third, there seems to be a concerted effort, so far with some resistance, to restrict mention of different forms of fat to total fats, with a special focus on trans fats.
Trans fats: Why now so prominent?
The puzzle over the various types of fat did not start with drafts of the Political Declaration. On arrival at the April Moscow ministerial-level meeting preparatory to the New York summit, I was struck by the fact that the 'zero draft' of the Moscow Declaration presented for discussion (32), specified decreased consumption of fat and trans fats as aspects of a healthy diet, but made no mention of saturated fats, in a section whose loose phrasing seemed to suggest that its purpose was to reduce obesity. Salt reduction was emphasised, together with interventions to control tobacco and the harmful use of alcohol, in the context of cardiovascular disease. The paragraph including reference to fats was improved in the agreed Declaration (12), which states that healthy diets are low in saturated fats, trans fats, salt and sugar, and high in fruits and vegetables. This time, total fats vanished. The influential Lancet paper published at that time (11) also gave great emphasis to salt reduction, and also recommended consumption of foods low in saturated and trans fats, omitting total fats, without giving any explanatory reference.
All this seemed odd. As indicated above, recommendations solidly based on a mass of evidence have for well over thirty years specified that in countries whose food systems are industrialised, consumption of both total fats and saturated fats should be reduced, and they also quantify what this means (2,3). Beginning almost thirty years ago, reports also identified trans fats as equivalently harmful to saturated fats (33) or quite possibly more so (3). There is no serious doubt that both trans fats and salt, consumed in typical quantities in industrialised diets, are important causes of cardiovascular disease. But what is the reason for their very special emphasis? And what was the reason for the curious omission of saturated fats from the 'zero draft' Moscow Declaration, and now their virtual or possibly total disappearance from the final Political Declaration?
Follow the money
One reason is easy to identify. The transnational food product manufacturers need to claim that left to their own devices they can be leaders in finding solutions to pandemic non-communicable diseases. They know that unless they show willing, sooner or later the pressure to impose statutory restrictions on their activities will become irresistible. So some time ago, probably beginning in 2007 when they were warned to expect legislation if they did not respond, they got together and decided that what they would offer was product reformulation that included use of somewhat less salt, and substantial reductions in trans fats.
Why, is because these moves are relatively easy. If the dominant food processors gradually reduce the salt in their products, consumers will get used to this, and – as far as it goes – that's good, of course. If they sharply reduce trans fat content, without affecting attractive qualities, that sounds good also. The deal was commercially attractive too, because in return for making these changes, industry can and does boast about them in prominent lettering on labels, giving the impression that the products are positively healthy. Often they are not. An energy-dense fatty salty snack containing a modest amount less salt, is still an energy-dense fatty salty snack.
But from the public health point of view, there are snags. As mentioned, if somewhat less salty snack products are advertised with health claims, and their sales continue rapidly to increase in lower-income countries, the net result could well be greater consumption of salt. Another snag is that trans fats are generated industrially by use of the partial hydrogenation process. The most economical way to eliminate trans fats is by more intense hydrogenation, which generates greater saturation of fats, or else by greater use of the highly saturated palm oil as a substitute.
So the food processing industry has a powerful motive to emphasise the dangers of trans fats and to keep quiet – and keep others quiet – about the dangers of saturated fats. An effective way to achieve this is by means of 'partnerships' involving negotiations which result in the disappearance of any mention of saturated fats from recommendations on healthy diets. It would be altogether too crude to suggest that some sort of deal to conceal has been agreed. But if saturated fats are indeed an important cause of cardiovascular disease, as has been maintained by virtually all expert groups going right back to the 1960s, the result of omitting the need for policies and actions to reduce saturated fats in food supplies and thus diets would be a public health fiasco. So the issue is important.
The effects of reducing trans fats
The concept of 'best buys' involving product reformulation is obviously problematic. It does not follow that actions that are most convenient and least costly for food processors are for this reason those that are most in the interests of public health. This would follow only if the actions really did have a big net public health benefit. So what about reduction or removal of trans fats, without consideration of the implications for saturated fats? As far as I can see, the story is unclear.
The basis for the conclusion that removal of trans fats in isolation is good policy, evidently derives from long standing work in which the World Bank, the US Centers for Disease Control and Prevention (CDC) and later WHO, have been partners. Since the 1980s the World Bank has been assessing health policy and programme priorities in lower-income countries. One outcome has been a series of books published in 2006 (34). These are based on rigorous analyses. However, estimates of cost effectiveness internationally – for example for diabetes care and treatment (35) – while using what information is available from lower-income countries, have sometimes been based on US experience. The results of this work have been used as a basis for WHO policies as these have developed in recent years.
Walter Willett of Harvard was asked to head the project for the chapter on diet and the prevention of non-communicable diseases (36). This could be seen as a surprising choice, because the Harvard School of Public Health group of which he is the head investigator is famous for its rejection of much of the mainstream thinking of WHO and indeed the US Institute of Medicine's conclusions on nutrition and the determinants of NCDs. In particular, the Harvard group downplays the solid consensus judgement that saturated fats are an important cause of cardiovascular disease. The team for the project also included distinguished scholars from elsewhere in the US, and Pekka Puska from Finland.
As published, the chapter emphasised the dominance of trans fatty acids over saturated fats in altering the lipid pattern. This conclusion was in part based on Martin Katan's meticulous analyses of the stronger impact of trans rather than saturated fats on blood lipids in 60 metabolic lipid trials (37). The chapter also concluded that reduction of trans fats will of itself prevent cardiovascular disease. This is based on Harvard prospective studies on US nurses which show a correlation with trans fat estimates but not with saturated fat intakes and heart disease (38). On this basis, and given that it is not difficult to eliminate trans fats from food products, the chapter concluded that reduction of trans fats is of itself a cost-effective and valuable public health measure that should be given priority. There are though no trials testing the effect of reduction or elimination of trans fats on future cardiovascular disease. Such evidence would be robust, but the Harvard group considers that the evidence on trans fats is so solid and that trans fats are so toxic, that any such trials would be unethical (39).
Box 3
Trans fats: Slim evidence from 14 Pakistanis
A letter from the Harvard School of Public Health team published in the British Medical Journal in 1996 (40) asserts, in support of the policy to emphasise trans fats, 'In many developing countries, trans fat consumption is high because partially hydrogenated soybean oil is among the cheapest fats available. In South Asia, vegetable ghee, which has largely replaced traditional ghee, contains approximately 50 percent trans fatty acids'.
In support, the letter sets out findings that in 14 Pakistani consumers of hydrogenated vegetable ghee, the multiple forms of trans fatty acids, measured carefully in the US by gas liquid chromatography in adipose tissue samples, were about 50 per cent higher than in those eating non hydrogenated vegetable oils. The authors also claim that 50 per cent of the vegetable oils are in the form of trans fatty acids in poor countries such as India and Pakistan. They offer no evidence for this, except to assert in an earlier paper that vegetable oils in India could contain up to 60 per cent trans fats. However, a closer look at the data displayed in the BMJ letter shows that the trans fatty acid content is actually 4.99 per cent of the total fatty acid content in the adipose tissue of the 14 Pakistanis who were so-called high consumers of hydrogenated vegetable ghee.
This compares with a more robust study of total trans fatty acid status in 51 US subjects who had an almost identical average fat biopsy trans fat content of 4.7 per cent (41). However, their corresponding dietary assessment (albeit based on food frequency questionnaires) was 2.44 grams/day or 5 per cent of the total fat content of their diet. These data strongly suggest that the Karachi men consuming hydrogenated vegetable ghee were not on a higher intake than those in the US, and certainly were not on a fat intake of even 10 per cent trans fat.
This, is not to deny the value of removing industrially generated trans fatty acids from food supplies, but it illustrates how limited and indeed flawed are some of the apparently supportive data.
The conclusions of the World Bank/ CDC/ WHO project are, I surmise, the reason why mention of saturated fats, and even of total fats, in documents prepared for the UN summit, is so tentative, even to the point of disappearance.
There certainly is good biological evidence supporting the conclusion that trans fats should be sharply reduced. They markedly interfere with the normal desaturation of essential polyunsaturated fatty acids to their prostanoids as well as inducing dyslipidaemia (42). Steen Stender and colleagues have published good data showing that high amounts of trans fats are contained in a variety of popular fast, baked and other foods sold in lower income countries as well as in Europe and the US (43). Given that it is relatively easy for food manufacturers to avoid the generation of trans fats in their products, in itself this policy probably is cost effective and valuable. .
However, the question then is, what do products with less or no trans fats contain instead? If the replacement ingredients are harmless, the reformulation is obviously desirable. But as mentioned, two alternatives to trans fats are a more intensive hydrogenation process that generates increased levels of saturated fats, or else the use of highly saturated palm oil (44). If saturated fat is harmless, this would not matter. But notwithstanding the emphasis of the Harvard team, the overwhelming evidence remains that saturated fat is an important cause of cardiovascular disease. I now turn to this point.
Saturated fats: A crucial cause of CHD
For around half a century now, public health policies designed to reduce rates of cardiovascular disease, in parts of the world whose food supplies are industrialised and rates of the disease have been high, have as a prime priority, included the reduced consumption of saturated fats. This implies reform of food systems so that food supplies contain lower levels of saturated fats. This specific policy has been supported by WHO for around thirty years, as reflected in series of expert WHO reports (2,3,45). As a consequence, in high-income countries food supplies have been reformed, people have been consuming less saturated fat, and rates of cardiovascular disease have decreased. There are a number of reasons for the generally large falls in rates of death from cardiovascular disease in high-income countries and settings, and it is generally agreed that reduced consumption of saturated fat is one of the reasons.
Some epidemiologists do not agree with this view. In particular, the group at the Harvard School of Public Health do not find a correlation between consumption of saturated fat and rates of heart disease in their very large Nurses and Health Professionals cohort studies, and therefore conclude in general that the relationship is very weak or does not exist. Any such conclusion is an error. It is rare to find such a correlation in any cohort study. This was noted many years ago by Ancel Keys in report on the classic Seven Countries Study of which he was the principal investigator (46).
Epidemiology and biology: both are needed
The reason, which does not lead to the conclusion of the Harvard group, is a reminder that it is usually unwise to draw public health conclusions only from epidemiological findings. To be a reliable basis for public health recommendations, evidence normally needs to include consistent epidemiological and biological findings. As Keys and colleagues noted over 45 years ago, in a paper that should be better known (47), under strict metabolic conditions adults fed the same saturated fat intake show remarkable differences in their blood cholesterol responses. With individual baseline blood cholesterol levels, responses to changes in saturated fat can be predicted. It was not known at that time that these remarkable differences between individuals, which explain a substantial part of the usual skewed prevalence curve of cholesterol levels in a population, is genetically based. Joseph Goldstein and Michael Brown have shown (48) that the control of lipoprotein uptake by receptors in the liver to a large extent determine plasma lipoprotein concentrations. Regulation of the two principal chylomicron and lipoprotein hepatic receptor systems are now accepted as being markedly affected by genetic variation (49).
This genetic effect does not only occur in cases of homozygous and heterozygous hypercholesterolaemia, as some think. Around 60 per cent of the variation in plasma cholesterol levels in a population is genetically determined, with about 14 per cent of this variation being due to APO E polymorphisms (47). So it is no wonder that Ancel Keys and his colleagues found no relationship between saturated fat intake and heart disease in individuals, but a very clear relationship between individuals' blood cholesterol levels and the rate of coronary heart disease. This seems sometimes to be overlooked by investigators responsible for cohort studies. Some epidemiologists dismiss the relationship between levels of saturated fat consumption and of heart disease in different countries, as mere crude ecological correlations. But recognising these relationships in the context of the biological causal pathways of atherosclerosis made it clear that lipid-induced changes in cholesterol metabolism are the way by which saturated fatty acids induce the atherosclerosis responsible for the cardiovascular disease. This is illuminated by ecological studies, which suggest the overall magnitude of these effects.
To be really reliable as evidence, the findings from any one study team should be confirmed by that of others. Ancel Keys and his group undertook many meticulous metabolic studies showing that specific saturated fats induce increases in serum cholesterol levels (50). Their work has confirmed by similar metabolic feeding studies conducted a generation later by Mark Hegsted and colleagues (51), and more recently by Martin Katan and colleagues. Numerous subsequent cohort analyses have confirmed the relationship of blood cholesterol levels (and more specifically LDL cholesterol levels) to the development of coronary heart disease. All this explains and supports what until now is the universal policy of reducing dietary saturated fats consumption – and production – in order to lower the incidence and prevalence of cardiovascular disease. The policy springs from the science, it is rational, and it works.
Figure 2
Impact of reduced blood cholesterol on CHD mortality
Predicted and observed decline in CHD mortality
Data from Finland, 1972-2007 (52)

Figure 3
Impact of reduced saturated fats on blood cholesterol
Relative importance of different dietary components
Data from Finland, 1982-2007 (53)
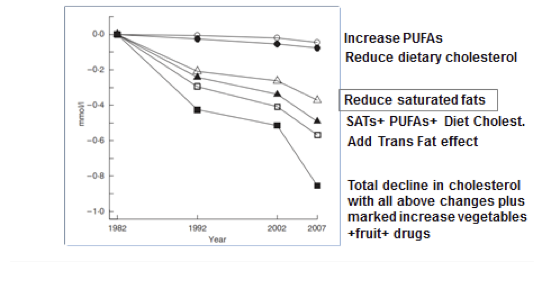
Perhaps the most important and significant work that has succeeded in reforming diets with the result of reducing rates and prevalence of cardiovascular disease, has been done in Finland, in continuous interventions and studies since the early 1970s. Some results of this work are shown in Figures 2 and 3, from papers both published last year, whose results are related. Figure 2 shows that the biggest contribution to the fall in cardiovascular disease between 1972 and 2007 has come about as a result of a steady drop in population average levels of blood cholesterol (52). Figure 3 shows that reduction in saturated fats has been far more important than other fatty acid changes, including a fall in trans fat intakes, in explaining the lower population cholesterol levels (53).
Trans fats and saturated fats: both important
This does not mean that trans fats are unimportant. For example, in Norway there has been as much as 15 grams a day of trans fat consumed as a result of the common use of modified fish oils. Policies that reduce saturated fats have also sharply reduced average trans fat intake which is now about 0.6 grams a day. In the same time period, saturated fat intakes fell by about 25-30 grams a day. If it is assumed that trans fats are twice as atherogenic as saturated fats, their reductions will have made equivalent contributions to the dramatic fall in the prevalence of heart disease in Norway (54).
There again though, the sharp rises in production and consumption of the very saturated palmitic acid from palm oil in countries such as Malaysia, India and China, which certainly has raised the blood cholesterol levels of these populations, will account for a substantial part of the increase in coronary heart disease in these countries. The traditional ghee made Indians susceptible, and still more saturated fat from other sources is a cause of heart disease rates that are now very high. Levels of trans fats in food supplies and diets do need to be reduced. So do levels of saturated fats. Rational public health policies must include both. Any policy that has the effect of lowering trans fats and raising saturated fats is likely to be injurious to public health.
Box 4
The ideal level of saturated fat intake
In 1982 the remarkable first '678' WHO report on cardiovascular prevention (45), in which Geoffrey Rose and Henry Blackburn played leading parts, set out the importance of reducing average, not just extreme, levels of serum cholesterol in populations, to protect against heart disease.
At that time seminal studies of Ancel Keys and his group from the Seven Countries metabolic epidemiological analyses were well known (46,55). These showed that blood cholesterol levels in Finland, Europe and the US were very high and were linked with coronary heart disease, whereas in Mediterranean countries and Japan blood cholesterol levels were low and corresponded with the prevailing low coronary heart disease levels.
The Seven Countries study identified smoking, hypertension and high levels of blood cholesterol (hypercholesterolaemia) as the three principal risk factors promoting coronary heart disease. Ancel Keys and his group also observed that low population levels of blood cholesterol were associated with low intakes of saturated fats. In later analyses of these studies they highlighted that high smoking rates and hypertension, such as in Mediterranean countries or Japan, could be associated with low CHD rates when cholesterol levels were very low. They concluded that dietary saturated fatty acid intake was crucial in making the impact of hypertension and smoking on CHD to evident. This finding, often now forgotten, has a reasonable basis, given current understanding of biology of atheromatous and other changes underlying coronary heart disease.
The '678' report specified a limit of 30 per cent of energy from fat. This was not because total fat had ever been shown to relate to coronary heart disease. The <30% total fat limit was a pragmatic goal, based on the idea that this should be a simple and effective way of reducing saturated fat intakes, then about 20 per cent of energy intake in high risk countries. The Seven Countries study showed, by finding that the Greeks studied had higher fat intakes and higher body mass indices (BMIs) but low coronary artery disease rates, that total fat was not relevant for coronary heart disease (46). However, given that in the US and UK total fat intakes were then over 40 per cent and saturated fat intakes 20 per cent or even more of dietary energy, it was logical for the '678'report to set a target for reducing total fat.
Why the targets specified?
Why the targets of less than 30 per cent for total fat and less than 10 per cent for saturated fat? Why those numbers? It was known at the time that there were then other parts of the world, such as in Africa, the Middle East and Asia, where saturated fat intakes were then well below 5 per cent and total fat intakes were 10-15 per cent. Coronary heart disease rates were then often so low as to be difficult to measure accurately. But in careful studies carried out in China, the relationship between CHD rates and blood cholesterol was still seen at exceptionally low levels This China/Cornell/Oxford study (56,57) showed an average of 14 per cent total fat intake with differences between different Chinese counties varying from 4 to 24 per cent. Similarly the Seven Countries data from Japan showed an average total fat intake of 14 per cent
Recent analyses in which I participated suggest fat intakes at that time were about 8 per cent in Thailand (58) and about 19 per cent in Jamaica (59). So the '678'report, noting that East African malnourished children on perhaps 2-4 per cent total fat diets were handicapped by having to eat vast amounts of starchy foods to have enough energy to gain weight, specified a lower limit for total fat of 15 per cent energy and a higher limit of 30 per cent. This has had very unfortunate consequences, as I explain in the main text below.
The lower the blood cholesterol level of any population the better. The Seven Countries study and the China/Cornell/ Oxford study showed this, decades ago. There is no reason to specify up to 10 per cent saturated fat intake, or up to 30 per cent total fat, as ultimate goals for optimum health. Lower levels consistent with adequate energy intake are healthy.
Figure 4
Saturated fat and mortality
10-year coronary mortality in men - Seven Countries study
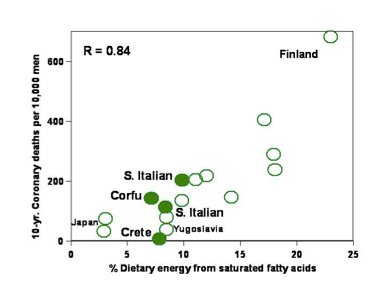
This figure, taken from the Seven Countries study, indicates that minimum intakes of saturated fats, around 5 per cent or less of energy, are optimum for heart health. It is true that Cretan men at that time had negligible coronary heart disease rates despite a 7 per cent saturated fat intake, but they were extremely physically active, working in mountainous countryside. Data from recent intervention studies with dietary change and the use of statins, show that the lower the LDL cholesterol – even below 2mmol/l, corresponding roughly to say 4mmol/l ( 155mg/dl) total cholesterol – the lower the risk of heart disease (60).
Fat: Total intakes remain important
My final comment is on all types of dietary fat – total fat in diets. This also has been minimised in the documents preparatory to the New York summit, almost to the point of only trans fats being identified among the 'best buys'.
This may be because the Harvard School of Public Health group considers that the contribution of total dietary fat to overweight and obesity is not significant, and instead, considers that carbohydrates with a high glycaemic index, including white rice and potatoes as well as sugary foods and drinks, are much more important as causes of obesity. One argument the Harvard group uses in support of their view, is that the results of trials designed to reduce weight that use lower-fat dieting regimes are unimpressive, or show no benefit. By contrast, Arne Astrup does see a relationship, albeit very modest, between reduction in fat intake (when specific energy intake levels are not set) and reduction in bodyweight (61).
However, trials in which various regimes are used to induce weight loss in overweight people are not a good basis for judgements about any dietary component. Characteristically they all have disappointing or even negative results, because of the adaptive biology during weight gain which then minimises the ease of weight reduction (62). Weight reduction trials are not a useful basis for determining dietary factors that induce weight increase. Other approaches are needed. Thus it was on the basis of metabolic studies, and cohort studies of general food patterns and physical activity, that the 2003 WHO '916' report (3) recommended diets rich in dietary fibre and low in energy density – and thus low in free sugars and also in fat – for weight stability.
Low-fat diets are vital for public health
The 1990 '797' WHO report Diet, Nutrition and the Prevention of Chronic Diseases (2) recommended on a world basis, diets including between 15-30 per cent energy from total fat, and between 0-10 per cent of saturated fat. It was not recognised at the time that policy-makers would interpret this recommendation as implying that any amount of total fat up to 30 per cent, and of saturated fat up to 10 per cent, of total energy, was optimum, and that saturated fat consumption of close to 10 per cent of energy could help to prevent coronary heart disease. This was unfortunate, most of all when this interpretation was applied to the diets of populations in lower-income countries which at that time on average contained amounts of total fats and saturated fats well under these levels.
The study group, which as mentioned I chaired, should also have questioned more forcefully the validity of the upper figure of 30 per cent fat and <10 per cent saturated fats. These values were not chosen in the modern ways as WHO now does, on a counterfactual basis as most likely to be protective, but were intermediate pragmatically chosen targets. The probable continuous relationship between fat intakes and both obesity and various common cancers from below 20 per cent to above 40 per cent did however mean that WHO, when considering obesity for its 2000 '894' report (19), stated that the right goal for fat might well be 20-25 per cent of energy.
Policy-makers have failed to address the need to configure food systems so that they contain only relatively low amounts of total fat and of saturated fat. This is having increasingly disastrous consequences. Rates of obesity, diabetes, cardiovascular disease and common cancers have risen rapidly, continue to do so, and are out of control, most of all in lower-income and impoverished parts of the world (63).
It is only fairly recently that the world's leaders have agreed a sound policy on tobacco control. They also have agreed policies on poverty reduction, in the Millennium Development Goals. The sure signs now are that this month's summit in New York on the prevention and control of non-communicable diseases will result only in an agreed statement of principles. Perhaps this is just as well. If the final Political Declaration was concrete, but its recommendations on food and nutrition had focused mainly on 'best buys' such as salt and trans fats, it would have been a massive failure of policy making. It would have had at best only small benefits and by ignoring crucial determinants of disease would also have had ill-effects. It would not have addressed the world crisis we are confronted with now.
Conclusion: So what now?
Reviews and commentaries that are preludes to events not yet occurred, typically end with recommendations designed to influence the nature and outcomes of these events. In the case of prevention and control of epidemic and pandemic non-communicable diseases, this was the purpose of the important Lancet paper published in April this year (11). But I am not going to follow suit. Now is far too late. The dice have been cast, the runes have been read. It is now pretty obvious that the summit will conclude with a Political Declaration confined to general principles
Comments published after the 20th of this month are likely to quote the Roman satirist Horace saying 'The mountains laboured, and out issued a ridiculous mouse'. This would not be altogether fair. A meeting held at ministerial rather than head of state and government level is not designed to agree new policies, like for example the Millennium Development Goals. We know that pandemic chronic diseases amount to a global crisis, that they have social, economic and environmental as well as behavioural and biological determinants, and that they can be prevented and controlled only by concerted action involving all appropriate actors. It is not a trivial achievement to have this agreed at the UN General Assembly, at a time in history when government leaders have much else on their minds. The task now is to translate general principles into policies and actions at continental, regional and national level.
We in our profession need to play a leading and guiding part in this work. So we must look ahead. I support the position of the World Public Health Nutrition Association, of which I am a founder and a Council member, contained in the Association's letter to UN secretary-general Ban Ki-moon, sent on 25 August (64) (available here as a pdf). This states that a modest outcome to the New York summit, and a general Declaration of commitment, needs to be seen as a first stage and not as a failure. Any general conclusion that the process has failed, and worse that it should not be attempted again, would benefit only those who gain by the abandonment of world affairs to 'the market', which everybody should know has failed.
Proper progress towards prevention and control of non-communicable diseases will be possible only when all actors realise that truly rational and sustainable food systems should be in the interests of industry as a whole. At the moment, as I see it, the food manufacturers and processors are thinking short-term. They imagine that better health means less wealth for them. So they are hostile. What's needed now is development of fuller analyses. These will show that the food industry as a whole can and will prosper while also playing its crucial part in protecting and promoting global health, of humans and of the living and physical world.
Key leaders of industry need to see and believe this, and show courage and imagination. There are precedents, for example in the electronic communications industries, whose outstanding leaders have strategic vision and whose products have transformed human capacities. There will be losers as well as winners, which is the nature of fair competition. This does not apply to the alcohol industry, any more than it does to the tobacco industry. But what we need now is to envision food systems whose products are beneficial to health and to society and the environment, as well as to speculators and shareholders.
As Association president Barrie Margetts has commented: 'The main message, which we need to take on board now, is that we need to regroup so as to be more persuasive and more effective. This must engage us, as professionals and citizens'. I agree. He also points out that 'There are also some good reasons to regroup and rethink. There are a number of crucial issues not properly addressed so far, one of which is how to control and prevent undernutrition and deficiencies at the same time as obesity and other chronic diseases. Governments of impoverished countries don't have the resources or often the inclination to try to control non-communicable diseases in isolation'. I agree.
Any medicalised approach to disease management is hopelessly unrealistic for lower-income regions and countries. I say this as a qualified physician who has practiced medicine for many years, and who has worked in several materially poor countries in Latin America, the Caribbean, Africa and Asia, personally or on a collaborative basis. What is needed, are coherent strategies that appropriately engage all actors, and that will effectively address what is now the appalling crisis of pandemic disease and disability. Thus, the population explosion, amplified by longer human life-spans, climate change, and resource depletion including water shortage, needs to be factored into plans for what will amount to a radically different system of global food systems. Food manufacturing industries should continue to flourish. But the environmental argument, that their products need to be based on compositions harmonious with the traditional and established food systems of Asia, Africa and Latin America, is overwhelming.
New background papers and general statements now need to be prepared. The draft Political Declaration states several times that disease and well-being has social, economic and environmental as well as biological and behavioural determinants. Indeed so. The implications of this insight need to be fully included and considered. For example, the draft Declaration has nothing to say about population growth. It also says nothing about the impact of epidemic non-communicable diseases, and of their prevention and control, on industry as a whole, or on the food industry as a whole – which includes primary producers – or on rural economies. These omissions, some spectacular, are listed in the editorial accompanying this commentary.and are referred to by colleagues in the series of 11 short commentaries in this issue of WN. They are a consequence of too much pressure and not enough insight or time.
The need to think and act strategically
To succeed, any journey to a summit needs to be inspired by vision of the big picture. Travellers who trudge despondently, heads down, will not see their goal or achieve their mission. The vision I share with very many colleagues, includes the following.
We all individually come to realise that our most precious possession is our own good health, for our own sake, and that of our family, community, and the work we do. In exactly the same way, the health of nations is more valuable than the wealth of nations. Besides, without health, wealth is jeopardised. This is why the protection and preservation of public health, which does indeed need to be economically viable, is a grand endeavour. The prevention and control of non-communicable diseases, by means that also reduce the burden of infectious and deficiency diseases, is indeed crucially important and urgent. But the work cannot succeed in isolation. The context is crucial. Diseases and disabilities that suddenly become epidemic and even pandemic, are sure warning signs of political and societal failure and breakdown. In this respect, rocketing rates of early-life obesity and diabetes are a global crisis that is inseparable from and needs to be coupled with the linked food, fuel and financial crises that now rightly preoccupy governments.
So new paths need to be laid down and trod, towards a properly informed and resourced journey to a new meeting that really is a summit, at head of state and government level. This will take time. So be it. An initial agreement to be made is that all parties to the meeting must have interests that are consistent with those of public health. Conflicted industry should be engaged in the process, but in the implementation of policy and not in its formulation. This will benefit industry as a whole, as well as being in the public interest. Here follow some further thoughts, for work to be done now.
Legislative and regulatory action with specified two to three year time limits should be given for radical changes in the composition of processed food and drink products. There must now be no argument about the need for statutory limitation of advertising and marketing of food and drink products to children and indeed to adolescents. More generally, the lessons of tobacco and alcohol control need to be learned. Measures of penalising by taxes and other formal methods need to be used to restrict the advertising and marketing of processed energy-dense products high in fat, sugar and salt, and sugared drinks, to adults as well as to children and adolescents. Corresponding legal and fiscal encouragement needs to be given to all industry sectors whose products are healthy. All institutions and places funded with public money should set a time line whereby all foods and drinks of whatever nature should conform to progressive specified and legally binding standards.
We need to move towards a new period of human history. This is of a time when preoccupation with disease, at personal, family, community, national and global levels, no longer clouds our vision. It will be a time when fear of premature disability and suffering no longer thwarts the personal, social, economic and environmental aims and ambitions that we share, in our determination to sustain our lives, that of the generations that will succeed us, and life on our planet.
There is much to do.
References
- Draft Political Declaration of the High-Level Meeting on the Prevention and Control of Non-Communicable Diseases. Draft of 29 July. Pdf available here
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a WHO study group. WHO technical report series 797. Geneva: WHO, 1990.
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a joint WHO/FAO expert consultation. Geneva: WHO, 2003.
- Ezzati M, Lopez A, Rodgers A et al. Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360: 1347-1360.
- WHO. Global Health Risks. Mortality and burden of disease attributable to selected major risks. Geneva: WHO, 2009.
- CARICOM. Summit of CARICOM Heads of Government on Chronic Non- Communicable Diseases. Stemming the Tide of Non-Communicable Diseases. Executive summary. Port of Spain, Trinidad, 2007. Pdf available here
- NCD Alliance. www.ncdalliance.org. NCD priority statement: see: http://www.ncdalliance.org/sites/default/files/resource_files/Lancet%20and%20NCD%20Alliance%20Priority%20NCD%20Interventions.pdf.
- WHO. Principles and recommendations for interaction between WHO secretariat and the alcohol industry. ADG/NMH to regional directors, ADGs. Internal memorandum, 10 July 2006. Pdf available here.
- McMichael AJ, Butler C. Promoting global population health while constraining the environmental footprint. Annual Reviews of Public Health 2011, 32, 179-197.
- World Health Organization. Global Status Report on Non-Communicable Diseases 2010. Geneva: WHO, 2011. Pdf available here.
- Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. The Lancet DOI:10.1016/50140-6736(11)603930. Published on-line on 6 April 2011. Pdf available here.
- First Global Ministerial Conference on Healthy Lifestyles and Non-communicable disease control. Moscow Declaration. 29 April 2011. Pdf available here.
- World Health Organisation. Global Strategy on Diet, Physical Activity and Health. Geneva: WHO, 2004.
- World Health Organization. 2008-2113 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva: WHO, 2008.
- World Health Organization. Global Strategy to Reduce the Harmful Use of Alcohol. Geneva: WHO, 2011.
- World Health Organization. Targets to monitor progress in reducing the burden of noncommunicable diseases. Recommendations from a WHO targets working group. Geneva: WHO, 15 July 2011. Pdf available here.
- Rehm J, Mathers C, Popova S et al. Global burden of diseases and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet 2009; 373, 9862: 2223-2233.
- World Health Organization. Global Status Report on Alcohol and Health. Geneva: WHO, 2011. Available at: http://www.who.int/substanceabuse/publications/global alcoholreport/en/
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO consultation. Technical report series 894. Geneva: WHO, 2000.
- Anon. Urgently needed: a Framework Convention for obesity control. [Editorial]. The Lancet 2011, 378, 9793: 712.
- Swinburn B, Sacks G, Hall K et al. The global obesity pandemic: shaped by global drivers and local environments. The Lancet 2011, 378, 9793: 804-814.
- Gortmaker S, Swinburn B, Levy D et al. Changing the future of obesity: science, policy, and action. The Lancet 2011, 378, 9793: 838-847.
- Prentice A, Jebb S. Fast foods, energy density and obesity: a possible mechanistic link. Obesity Reviews 2003, 4, 4, 187-194.
- Stubbs J, Ferres S, Horgan G. Energy density of foods: effects on energy intake. Crit Rev Food Sci Nutr 2000, 40, 481-515.
- World Cancer Research Fund/ American Institute for Cancer Research. Food, Nutrition, Physical Activity and the Preventjon of Cancer: A Global Perspective. Washington DC: AICR, 2007.
- Capuccio F, Capewell S, Lincoln P, McPherson K. Policy options to reduce spopulation salt intake. British Medical Journal 2011; 343, d4995 DOI:10,1136bmj.d4995.
- Cohen D, Farley T. Eating as an automatic behavior. Prev Chronic Dis 2008; 5, 1. http://www.cdc.gov/pcd/issues/2008/jan/07_0046.htm.
- Institute of Medicine of the US National Academies of Science. Food Marketing to Children and Youth: Threat or Opportunity? Washington DC: IOM, 2005.
- Hwang K, Velanova K, Luna B. Strengthening of top-down frontal cognitive control networks underlying the development of inhibitory control: a functional magnetic resonance imaging effective connectivity study. Journal of Neuroscience 2010; 30: 15535-15545.
- Bava S, Tapert S. Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychology Reviews 2010 ; 20: 398-413.
- Dosenbach N, Nardos B, Cohen A, et al. Prediction of individual brain maturity using fMRI. Science 2010, 329, 1358-1361. Erratum in: Science 2010; 330: 756
- First Global Ministerial Conference on Healthy Lifestyles and Non-communicable disease control. Zero Draft Moscow Declaration. 29 March 2011.
- Department of Health and Social Security. Diet and Cardiovascular Disease. Committee on Medical Aspects of Food Policy. Report 28. London: HMSO, 1984.
- World Bank/ Centers for Disease Control and Prevention/ World Health Organization Disease Control Priorities Project see: http://www.dcp2.org/page/main/Home.html
- Venkat Narayan K, Zhang P, Kanaya A et al. Diabetes: the pandemic and potential solutions.[Chapter 30] In: Disease Control Priorities in Developing Countries (2nd Edition). New York: Oxford University Press, 2006. DOI: 10.1596/978-0-821-36179-5/
- Willett W, Koplan J, Nugent R et al. Prevention of chronic disease by means of diet and lifestyle changes. [Chapter 44] In: Disease Control Priorities in Developing Countries (2nd Edition). New York: Oxford University Press. DOI: 10.1596/978-0-821-36179-5/
- Mensink R, Zock P, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. American Journal of Clinical Nutrition 2003, 77, 1146-1155.
- Sun Q, Ma J, Campos H, et al. A prospective study of trans fatty acids in erythrocytes and risk of coronary heart disease. Circulation. 2007 ;115:1858-1865.
- Willett W, Ascherio A. Trans fats: are the effects only marginal? American Journal of Public Health 1994; 84, 722-724.
- Ascherio A, Cho E, Walsh K, et al. Premature coronary deaths in Asia [Letter]. British Medical Journal
- Lemaitre R, King I, Patterson R, et al. Assessment of trans-fatty acid intake with a food frequency questionnaire and validation with adipose tissue levels of trans-fatty acids. American Journal of Epidemiology 1998; 148, 1085-1093.
- Wahle K, James WPT. Isomeric fatty acids and human health. European Journal of Clinical Nutrition 1993, 47, 828-839.
- Stender S, Dyerberg J, Astrup A. High levels of industrially produced trans fat in popular fast foods. New England Journal of Medicine 2006, 354:1650-1652.
- Stender S, Astrup A, Dyerberg J. What went in when trans went out? New England Journal of Medicine 2009, 361, 314-316
- World Health Organization. Prevention of Coronary Heart Disease. Report of a WHO expert committee. Technical report series 678. Geneva: WHO, 1982.
- Keys A. (ed). (1980) Seven Countries. A Multivariate Analysis of Death and Coronary Heart Disease. Cambridge, MA: Harvard University Press, 1980.
- Keys A, Anderson J, Grande F., Serum cholesterol response to changes in the diet III. Differences among individuals. Metabolism 1965; 14: 766-75
- Goldstein J, Brown M. The LDL receptor. Arterioscler Thromb Vasc Biol 2009, 29, 431-438
- Davignon J, Gregg R, Sing C. Apolipoprotein E polymorphism and atherosclerosis. Arteriosclerosis 1988 ;8: 1-21.
- Keys A, Anderson J, Grande F. Serum cholesterol response to changes in diet IV Particular saturated fatty acids in the diet. Metabolism 1965; 14: 776-786.
- Hegsted D, Ausman L, Johnson J, Dollal G. Dietary fat and serum lipids: an evaluation of the experimental data. American Journal of Clinical Nutrition 1993; 57: 875-883
- Vartiainen E, Laatikainen T, Peltonen M, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. International Journal of Epidemiology 2010 ; 39:504-518
- Valsta L, Tapanainen H, Sundvall J, et al. Explaining the 25-year decline of serum cholesterol by dietary changes and use of lipid-lowering medication in Finland. Public Health Nutrition 2010; 13: 932-938
- Pedersen J, Tverdal A, Kirkhus B. Diet changes and the rise and fall of cardiovascular disease mortality in Norway. Tidsskr Nor Laegeforen. 2004, 124: 1532-1536.
- Keys A. Overweight, obesity, coronary heart disease, and mortality: the W.O. Atwater Memorial Lecture, 1980. Prog Clin Biol Res. 1981 ;67: 31-46.
- Chen J, Campbell T, Li J, Peto R. Diet, Lifestyle and Mortality in China. Oxford: Oxford University Press, Cornell University Press, and People's Medical Publishing House, 1990.
- Peto R, Boreham J, Chen J, Li J, et al. Plasma cholesterol, coronary heart disease, and cancer. British Medical Journal.1989; 298: 1249.
- James WPT, Rojroongwasinkul N, Rikshasuta T et al. Food imports and dietary change: a perspective from Thailand. In: Hawkes C, Blouin C, Henson S et al (eds). Trade, Food, Diet and Health Perspectives. Oxford: Wiley Blackwell, 2010.
- See FAO food balance sheets at http://faostat.fao.org/site/
- Cholesterol Treatment Trialists' Collaboration. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. The Lancet 2010 ; 376: 1670-1681
- Astrup A. The role of dietary fat in obesity. Semin Vasc Med. 2005; 5:40-47.
- Rosenbaum M, Goldsmith R, Bloomfield D, et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. Journal of Clinical Investigation 2005 ;115: 3579-3586'
- Astrup A, Dyerberg J, Selleck M, Stender S. Nutrition transition and its relationship to the development of obesity and related chronic diseases. Obesity Reviews. 2008 ; 9 Suppl 1:48-52.
- Anon. The Association writes to Ban Ki-moon. World Public Health Nutrition Association website, September 2011. Available at: www.wphna.org
Acknowledgement and request
Readers are invited please to respond. Please use the response facility below. Readers may make use of the material in this editorial if acknowledgement is given to the Association, and WN is cited
Please cite as: James WPT. UN Summit on non-communicable diseases. Up to the Summit: Inglorious paths.[Commentary] World Nutrition, September 2011, 2, 8: 352-399. Obtainable at www.wphna.org
The opinions expressed in all contributions to the website of the World Public Health Nutrition Association (the Association) including its journal World Nutrition, are those of their authors. They should not be taken to be the view or policy of the Association, or of any of its affiliated or associated bodies, unless this is explicitly stated.
WN commentaries are subject to internal review by members of the editorial team.
I would like to pay tribute to the huge effort put in by Geoffrey Cannon, in first checking the sequence, significance and content of all the myriad drafts of the documents relating to the preparations for the Summit, and also for highlighting omissions of mine which we had discussed but I had not included. His work then to reorder my various sections and to edit the whole comment appropriately is a rare commitment which improved my attempts to develop a logical and understandable story through, on what was inevitably an extremely tight schedule. I am very grateful.
I am president of the International Association for the Study of Obesity, and the founder and first director of the International Obesity Task Force. From 1982 to 1999 I was director of the Rowett Research Institute. I was a member of the panel responsible for the 1984 COMA report on cardiovascular disease, chair of the study group responsible for the 1990 WHO '797' report on diet, nutrition and the prevention of chronic diseases, a member of the secretariat responsible for the 2000 WHO '894' report on obesity, a member of the panel responsible for the 2003 WHO '916' report on diet, nutrition and the prevention of chronic diseases, and a member of the panel responsible for the 2007 WCRF/AICR report on cancer prevention.